
18) Spinal Disc Herniation: A Physiotherapist’s Guide to Protect and Recover
Back pain is something most of us will experience at some point in life, and one of the more common culprits is a spinal disc herniation. It sounds dramatic, but don’t worry – while it can be painful and even scary when it causes nerve symptoms, physiotherapy plays a huge role in recovery. In fact, many people get better without needing surgery, even in cases where it initially seems like an option.
In this blog, we’ll break down what a spinal disc herniation is, why it happens, common symptoms, and how physiotherapy can help. We’ll also share a real-life case of a patient who was initially referred to a neurosurgeon but ended up avoiding surgery with a solid physiotherapy plan.
What is a Spinal Disc Herniation?
Your spine is made up of 24 vertebrae, stacked up like building blocks. Between these vertebrae are little cushions called intervertebral discs, which act as shock absorbers and help keep everything moving smoothly.
Each spinal disc has a soft, jelly-like centre (nucleus pulposus) and a tougher outer layer (annulus fibrosus). A spinal disc herniation occurs when the inner jelly pushes through a tear or weak spot in the outer layer. This can irritate nearby nerves, causing pain, numbness, tingling, or even weakness in the arms or legs, depending on which part of the spine is affected.
Why Do Disc Herniations Happen?
Herniated discs are usually the result of gradual wear and tear, known as disc degeneration. Over time, our discs lose some of their water content, making them less flexible and more prone to tearing or rupturing, even with minor strains or twisting movements. However, certain factors increase the risk:
- Aging – The older we get, the more our discs wear down.
- Repetitive Movements – Jobs or sports that involve a lot of bending, lifting, or twisting can add stress to the discs.
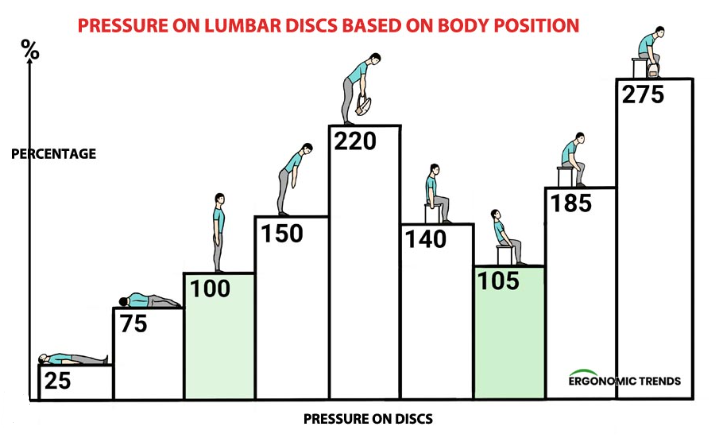
- Poor Posture – Sitting for long periods, especially with bad posture, can increase disc pressure.
- Lack of Exercise – Weak core and back muscles mean the spine gets less support.
- Heavy Lifting – Incorrect lifting techniques put excessive strain on the lower back.
- Smoking – Reduces blood flow to the discs, speeding up degeneration.

Symptoms of a Spinal Disc Herniation
The symptoms depend on where the spinal disc herniation occurs:
Lumbar Spine (Lower Back)
- Pain in the lower back, buttocks, and legs (often one side more than the other)
- Sciatica – shooting pain down the leg, sometimes into the foot
- Numbness, tingling, or burning sensations
- Muscle weakness in the leg or foot
- Difficulty standing, walking, or sitting for long periods
Cervical Spine (Neck)
- Neck pain, sometimes radiating into the shoulders and arms
- Numbness, tingling, or weakness in the arms or hands
- Headaches
- Limited range of motion in the neck
If the compression is severe, it can even lead to bowel or bladder dysfunction – a medical emergency known as cauda equina syndrome.
Physiotherapy: The Key to Recovery
Many people fear they’ll need surgery for a spinal disc herniation, but in most cases, conservative management (like physiotherapy) is incredibly effective. Here’s how physio helps:
1. Pain Relief and Symptom Management
- Manual Therapy: Hands-on techniques such as joint mobilisations, soft tissue massage, and myofascial release can help reduce muscle tension, improve joint mobility, and relieve nerve irritation. These techniques are particularly effective in easing pain and restoring function in the early stages of recovery.
- Taping & Bracing: In some cases, taping or bracing can help provide external support to reduce strain on the affected area. This can be useful in the acute phase of injury or when specific movements need to be restricted to allow healing. We personally stock the Immostrap back brace from Enovis, we have trialled many different braces over the years and we keep coming back to this one as it does the best job of deloading the spine in the acute phase only.
https://enovis-medtech.eu/en_US/Immostrap-74340.html
- Education: Understanding how to manage pain effectively is crucial. Physiotherapists provide guidance on posture, ergonomics, activity modifications, and pain relief strategies such as heat or ice application. This knowledge empowers patients to take control of their recovery.
2. Restoring Movement and Strength
- McKenzie Exercises: A specialised form of exercise therapy that focuses on repeated movements or sustained postures to help centralise pain and relieve nerve compression. These exercises are particularly beneficial for those with disc-related sciatica.
- Core Strengthening: Strengthening the deep stabilising muscles of the core helps offload stress from the spine, reducing the likelihood of further injury. Exercises such as planks, bird-dogs, and pelvic tilts are commonly used to build core endurance and support spinal stability.
- Stretching & Mobility Work: Stretching tight muscles (such as hamstrings, hip flexors, and lumbar paraspinals) and improving spinal mobility can help alleviate stiffness and promote more natural movement patterns. This reduces compensatory movements that might contribute to pain and dysfunction.
3. Addressing Underlying Causes
- Postural Training: Poor posture can contribute to ongoing spinal stress and discomfort. Physiotherapists work with patients to improve posture in daily activities, including sitting, standing, and lifting mechanics, to reduce excessive strain on the discs.
- Workplace Ergonomics: Many people spend hours at desks or in repetitive job roles that contribute to back pain. Physiotherapists offer ergonomic assessments and modifications, such as chair adjustments, monitor positioning, and movement breaks, to prevent future flare-ups.
- Gradual Return to Activity: A structured return-to-work or sports program ensures that the patient builds strength and endurance without overloading the spine too quickly. Physiotherapists create progressive exercise plans tailored to individual needs, helping patients regain confidence and function in their everyday lives.
Case Study: Avoiding Surgery Through Physiotherapy
One of our recent patients, let’s call him Mark, came to us with severe lower back pain as a result of a spinal disc herniation and worsening leg weakness. He had been struggling for months and was initially sent for a neurosurgeon opinion because his symptoms suggested nerve compression that might need surgery.
Mark had significant weakness in his leg, making it hard to walk properly. The neurosurgeon was concerned but suggested continuing physiotherapy for a few more weeks before deciding on surgery. We took that opportunity and worked on reducing his symptoms and improving his strength through targeted physiotherapy.
Over time, his pain decreased, his leg strength improved, and he regained confidence in his movement. Now, Mark trains at Plus Fitness in Frenchs Forest, focusing on strengthening his back and core to prevent future issues. He’s thrilled with his outcome, and best of all – no surgery was needed!
When is Surgery Necessary?
While physiotherapy is effective for most cases, some situations do require surgery. Surgery may be considered if:
- Symptoms persist despite months of conservative treatment
- There’s significant muscle weakness that worsens over time
- There’s loss of bowel or bladder control (cauda equina syndrome)
- The pain is so severe it affects quality of life
Spinal disc herniation surgery, also called a discectomy, removes the herniated part of a spinal disc. The goal is to relieve pressure on the nerves. Fortunately, these cases are the minority, and most people improve with a solid rehab plan.
Final Thoughts
A spinal disc herniation might sound like a big deal, but it doesn’t have to mean surgery. With the right physiotherapy approach, many people recover fully and return to their normal activities without going under the knife. If you or someone you know is struggling with back pain or sciatica, don’t wait – getting assessed early can make all the difference.
Need help? Book in with X Physio physio today and start your journey to a stronger, pain-free back! Our number is 9806 3077.
References
- Physiopedia. “Intervertebral Disc Herniation.” Available at: https://www.physio-pedia.com/Intervertebral_Disc_Herniation
- Spine-Health. “Herniated Disc Treatment.” Available at: https://www.spine-health.com/conditions/herniated-disc/herniated-disc-treatment
- Australian Physiotherapy Association. “Managing Back Pain.” Available at: https://australian.physio/injury-list/back-pain



