Injury slowing you down? The right recovery plan can make all the difference. From early movement to expert hands-on physio, this blog covers the best things you can do to bounce back better. We’ll also share a recent patient story that proves just how effective physiotherapy can be.
Introduction: Injury Recovery Doesn’t Have to Be a Mystery
Whether it’s a dodgy ankle from footy, back pain from gardening, or a shoulder strain at work, getting injured can be frustrating. But good news—recovery doesn’t have to be slow, painful, or confusing. With the right strategies, support, and mindset, you can get back to your normal faster than you think.
In this blog, we’ll break down the best things you can do to help your body recover, from day one of the injury to those final stages of getting strong again. You’ll get practical tips backed by science and a real-world patient example to show it all in action.
Let’s dive in.
1. Respect the Injury—But Don’t Baby It
When something hurts, our natural instinct is to rest completely. While a short period of rest is important, doing nothing for too long can actually make things worse. The key is knowing when to rest and when to move.
Early Stage (0–72 hours): Follow the PEACE & LOVE Approach
You may have heard of R.I.C.E (Rest, Ice, Compression, Elevation). That’s a bit outdated now. The latest approach is PEACE & LOVE, and it’s far more holistic:
PEACE (first 1–3 days):
- P – Protect (avoid movements that cause more pain)
- E – Elevate the limb
- A – Avoid anti-inflammatories (they may slow healing)
- C – Compress (support the area with tape or bandage)
- E – Educate (learn what to do next—like reading this blog!)
LOVE (after 72 hours):
- L – Load the area gradually
- O – Optimism (your mindset matters!)
- V – Vascularisation (gentle aerobic activity to get blood moving)
- E – Exercise (guided, progressive rehab)

Tip: Don’t go it alone. A physio can help you find that sweet spot between doing too much and doing too little.
2. See a Physiotherapist Early
This one’s a game-changer. Many people wait weeks—or months—before seeing a physio. But early intervention helps identify the issue, start treatment, and prevent long-term problems.
A good physio will:
- Diagnose your injury properly
- Give you a clear plan of attack
- Use hands-on treatment to reduce pain and improve movement
- Teach you targeted exercises to speed up healing
- Help you prevent re-injury
Physiotherapy isn’t just about massages and stretches. It’s about functional recovery—getting you back to doing what you love.
3. Move Smart, Not Hard
Movement is medicine—when done right.
Once you’re past the initial inflammation, gentle movement helps reduce stiffness, improve circulation, and activate healing in the muscles, joints, and tissues. But jumping back into sport or gym workouts too soon can backfire.
Your physio will guide you through:
- Range of motion exercises
- Isometric loading (great for tendons)
- Functional movement drills
- Strength-building exercises tailored to your stage of recovery
Case in point: After a calf tear, walking laps too soon might cause a re-tear—but light banded foot pumps could promote safe healing.
4. Stay Consistent With Your Rehab Exercises
We get it—rehab exercises can feel repetitive. But they work if you do them. Research shows that compliance with physiotherapy exercise programs leads to significantly better outcomes (Kolt & McEvoy, 2003).
Here’s how to stay on track:
- Set reminders in your phone
- Link exercises to daily habits (e.g., after brushing your teeth)
- Use a printed or digital physio program to track progress
- Ask your physio to mix it up to keep it engaging

Real talk: Missing two weeks of rehab can undo a lot of progress.
5. Look After the Whole Body
Your body is a system, not a set of isolated parts. To recover fully, think big picture.
- Nutrition: Eat a balanced diet with protein, vitamins C and D, and omega-3s to fuel tissue repair.
- Sleep: Your body repairs itself while you sleep. Aim for 7–9 hours a night.
- Hydration: Water supports circulation and muscle recovery.
- Stress management: High stress can slow healing, so make time for rest, relaxation, and mindset work.

Fun fact: Studies show that being optimistic can improve physical recovery outcomes (Main et al., 2010).
6. Don’t Rely Solely on Pain Relief Meds
While over-the-counter medications can provide short-term relief, they don’t address the root cause. Relying too heavily on painkillers can also lead to delayed recovery and other health risks.
Instead:
- Use ice, heat, or taping as recommended by your physio
- Try gentle stretching and movement
- Learn pain education strategies to understand what’s safe vs. harmful pain
Remember: Pain is a signal, not a sentence. Learn what your body’s trying to tell you.
7. Gradually Return to Sport or Work
This is where many people go wrong—returning to full activity too fast. You might feel “okay,” but if your tissues haven’t regained full strength or coordination, re-injury risk is high.
A physio-guided return-to-play or return-to-work plan will include:
- Functional testing (e.g., single-leg hop test, lift test)
- Strength and stability benchmarks
- Sport-specific drills
- Load tolerance monitoring
It’s not just about being pain-free. It’s about being ready.
8. Reassess and Adjust Along the Way
Injuries are dynamic. What worked in week 1 might not be right for week 4. That’s why ongoing reassessment with your physio is so helpful.
Your treatment might shift to include:
- Advanced rehab techniques (e.g., reformer Pilates, neuromuscular re-training)
- Manual therapy to address stiffness or imbalances
- Education to help you become more confident in self-managing flare-ups
Recovery isn’t a straight line—but it is a team effort.
Patient Spotlight: Meet James
James, 42, came to our clinic after injuring his lower back while helping a mate move house. He tried to “push through” the pain at first, but after a week of poor sleep and difficulty bending, he finally came in.
On assessment, we found signs of a lumbar facet joint sprain, with muscle guarding and reduced trunk rotation.
Here’s how his recovery went:
- Week 1–2: Hands-on treatment for pain relief and mobility, plus light activation drills
- Week 3–5: Introduced core stability and glute strengthening exercises
- Week 6+: Returned to light gym sessions and work duties with modified loads
Now, James is pain-free, sleeping better, and back to playing touch footy on weekends. He’s still doing his strength program twice a week at Plus Fitness and even said, “Physio saved my back—and probably my sanity!”
To find out more about a lower back pain, read this blog.
Wrap-Up: Recovery Is a Process, But You’re Not Alone
Getting injured can be a setback, but it doesn’t have to be the end of the story. With the right strategies—like early physio, progressive exercise, and listening to your body—you can bounce back stronger.
Your next step? Book in with a physio who knows how to guide you through every stage of recovery.
Give us a call today on 9806 3077, or book online, just CLICK HERE
References:
- Dubois, B., & Esculier, J. F. (2020). PEACE & LOVE: A new approach to soft tissue injuries. British Journal of Sports Medicine. https://bjsm.bmj.com/content/54/2/72
- Kolt GS, McEvoy JF. (2003). Adherence to rehabilitation in patients with low back pain. Manual Therapy, 8(2), 110–116. https://doi.org/10.1016/S1356-689X(02)00156-X
- Main, C. J., George, S. Z. (2010). Psychological predictors of pain and disability. Clinical Journal of Pain. https://journals.lww.com/clinicalpain
Post surgery rehab plays a critical role in getting you back to doing what you love. Undergoing surgery is a major step—but it’s not the finish line. In this blog, we’ll explore how physiotherapy bridges the gap between the operating table and full recovery, and why skipping it can slow you down.
The Hidden Secret Behind a Successful Post Surgery Rehab
You’ve made it through surgery. The hard part’s over, right?
Not quite.
While surgery fixes the structural problem—like repairing a torn ligament or replacing a joint—it doesn’t magically restore strength, movement, or function. That’s where physiotherapy comes in. Without a solid rehab plan, your body won’t relearn how to move properly. Muscles weaken. Joints stiffen. Scar tissue can build up.
Post surgery rehab and Physiotherapy is the secret weapon to a full and lasting recovery.
Let’s unpack why it matters and how it can set you up for long-term success.

Why Is Physiotherapy After Surgery So Important?
1. Restores Range of Motion and Flexibility
During Post surgery rehab it’s common for the body to become stiff—especially if you’ve had to rest or wear a brace. Physios use manual therapy and specific exercises to gradually restore movement, reduce tightness, and help prevent joint contractures or long-term limitations.
🧠 Fun fact: Studies show that early mobilisation after surgery (when appropriate) can improve outcomes and reduce complications.
Source: National Library of Medicine
2. Rebuilds Strength the Right Way
Muscle loss (atrophy) happens quickly when you’re not using a limb post-op. Physiotherapists develop tailored strength programs that target weak or inhibited muscles—safely and progressively—without overloading healing tissues.
We’re not just aiming for strength. We’re aiming for balanced, functional strength that supports your everyday life or sport.
3. Reduces Swelling and Scar Tissue
Swelling and scar formation are part of the healing process—but too much of either can block progress. Physios use techniques like manual lymphatic drainage, massage, dry needling, and guided movement to reduce inflammation and break down adhesions.
This helps prevent complications like joint stiffness or frozen shoulder in post-op shoulder surgeries.
4. Retrains Movement and Prevents Compensations
The body is clever. After surgery, it finds new ways to move—often in ways that create problems down the track (like limping or favouring one side).
Post surgery rehab will help retrain normal movement patterns so your body doesn’t develop habits that could lead to further injury or pain. This is critical in hip, knee, ankle, shoulder, and spinal surgeries.
5. Gets You Back to Work, Sport and Life—Faster
Whether your goal is to return to soccer, play with your grandkids, or get back to work without discomfort, physiotherapy provides structure, accountability, and measurable goals along the way.
Plus, you’ll leave with strategies to avoid re-injury—because no one wants to go through surgery twice.

Common Surgeries That Benefit From Physiotherapy
If you’ve had (or are planning to have) one of these procedures, physio is non-negotiable:
- ACL Reconstruction
(Rehab can take 9–12 months, and structured strength work is key to avoiding re-injury.) - Total Knee Replacement
(Improving range of motion and quadriceps strength is critical to walking and stair climbing.) - Rotator Cuff Repair
(Gradual mobilisation is crucial to prevent frozen shoulder while protecting the repair.) - Hip Replacement
(Focus is on regaining balance, gait training, and hip stability.) - Spinal Surgery (e.g., laminectomy, discectomy, fusion)
(Movement retraining, core stability, and gradual loading of the spine are essential.) - Shoulder Stabilisation or Labral Repair
(Progressive rehab helps return to sport or overhead tasks with full function.)

Real Case Study: Rob’s Comeback After a Total Knee Replacement
Rob, a 67-year-old retired firefighter, came to our clinic six weeks after his total knee replacement. He had persistent swelling, difficulty bending the knee, and was struggling to walk comfortably—even with a frame.
He admitted, “I thought the hard part was the surgery. But I feel like I’m stuck.”
As part of his Post surgery rehab, we assessed:
- Knee range of motion
- Quadriceps activation
- Gait mechanics
- Swelling and pain levels
Here’s what we did for Rob:
✅ Manual therapy to reduce swelling and improve soft tissue mobility
✅ Gentle joint mobilisation to help knee flexion and extension
✅ Quadriceps activation drills using NMES (neuromuscular electrical stimulation)
✅ Progressive weight-bearing exercises to build strength and stability
✅ Education on home exercises, icing, elevation, and pacing strategies
Fast forward 3 months…
Rob ditched the walker, climbed stairs comfortably, and hit 120 degrees of knee flexion. He was even back to bushwalking with his wife—something he thought was off the cards forever.
“Physio helped me take the next step. Literally. I don’t think I would’ve progressed without it.”
For more information on knee replacements, have a read of our Knee Replacement Blog.
What Happens If You Skip Rehab?
Let’s be honest—surgery without post surgery rehab is like buying a car but never learning to drive it.
Without post-op physiotherapy, you may face:
🚫 Long-term stiffness or weakness
🚫 Poor movement patterns
🚫 Chronic pain
🚫 Higher risk of re-injury or additional surgeries
🚫 Delayed return to work or sport
What Does Post Surgery Rehab Look Like?
Here’s a typical flow:
🗓️ Early Phase (0–2 weeks)
- Pain relief and swelling control
- Gentle mobility (where appropriate)
- Education and protection strategies
- Isometric exercises
- Hydrotherapy (in some cases)
🏃 Middle Phase (2–8 weeks)
- Increase joint range and muscle activation
- Functional strength and balance
- Scar management
- Begin low-load cardio (e.g., cycling, walking)
🏋️ Advanced Phase (8–16 weeks)
- Higher level strength training
- Return-to-work or sport-specific movements
- Movement retraining and speed drills
- Addressing remaining limitations
🛡️ Final Phase (3–6+ months)
- Performance goals
- Injury prevention
- Independent gym or home program
Your post surgery rehab program will vary based on the type of surgery, your body, and your goals—but this gives you a rough idea of what to expect.

A Few Common Questions We Get Asked
💬 “How soon after surgery should I start physio?”
In many cases, straight away (or within a few days). Your surgeon and physio will collaborate on timing based on the procedure.
💬 “Do I really need ongoing sessions?”
Yes—rehab is not a one-session fix. Progress happens week by week, and consistency is key to regaining full function.
💬 “Isn’t walking enough?”
Walking is great—but it’s not enough to address strength deficits, mobility restrictions, or movement patterns. Your physio program targets those issues directly.
Final Thoughts: Your Recovery Is a Journey, Not Just an Event
Think of surgery as the reset. But it’s post surgery rehab that builds the new foundation.
If you’ve had surgery—or have one coming up—talk to a physio early. We’ll set realistic goals, reduce complications, and guide you through each step.
There’s no need to guess your way through recovery. We’re here to make sure your hard work (and your surgeon’s) pays off.
Need Help with Post surgery rehab?
Whether you’re recovering from a joint replacement, ligament repair, or spinal procedure, our team can help you bounce back stronger than ever.
Give us a call today on 9806 3077, or book online, just CLICK HERE
References & Further Reading
- Australian Physiotherapy Association – Physiotherapy After Surgery
- Healthdirect – Rehabilitation After Surgery
- Better Health Channel – Knee Replacement Recovery
- National Library of Medicine – Early Mobilisation in Surgical Patients
Dizziness can be a frustrating and even scary experience. Whether it’s a sudden spinning sensation, a feeling of unsteadiness, or general light-headedness, dizziness can interfere with daily life. The good news? Physiotherapists are trained to assess and treat the various types, including vertigo, to help you regain balance and confidence.
In this blog, we’ll explore how physiotherapy can help with dizziness, the different types that can be treated, and a real-life case of a patient who improved with physiotherapy.
Types of Dizziness Physiotherapists Can Assess and Treat
Dizziness isn’t just one condition—it’s a symptom with multiple causes. Physiotherapists can assess and treat:
1. Benign Paroxysmal Positional Vertigo (BPPV)
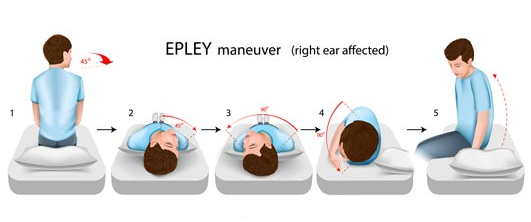
BPPV is one of the most common causes of vertigo. It occurs when tiny calcium crystals in the inner ear become dislodged and move into the wrong canal. This leads to brief but intense episodes where the world feels as though it is spinning. It is often triggered by head movements, such as rolling over in bed or looking up.
Physiotherapy treatment:
- Canalith repositioning manoeuvres (e.g., the Epley manoeuvre) to move the dislodged crystals back where they belong.
- Education on how to manage symptoms and avoid provoking movements until the issue is resolved.
2. Cervicogenic Dizziness
This type originates from the neck and is often linked to poor posture, neck stiffness, or injury (e.g., whiplash). People with cervicogenic dizziness often report feeling unsteady or “off-balance” rather than experiencing true vertigo.
Physiotherapy treatment:
- Hands-on treatment for neck stiffness and muscle tightness.
- Postural correction and strengthening exercises.
- Balance retraining to improve stability.

3. Concussion-Related Dizziness
It is a common symptom following a concussion. It may be due to vestibular dysfunction, neck issues, or visual disturbances.
Physiotherapy treatment:
- Vestibular therapy to improve gaze stability and balance.
- Neck treatment if cervicogenic is present.
- Graded return-to-activity programs to ensure safe recovery.

A Recent Patient Case: Overcoming Cervicogenic Dizziness with Physiotherapy
Let’s look at a real-life example of a patient who was able to improve with physiotherapy.
Meet Sarah (name changed for privacy)
Sarah, a 42-year-old office worker, came into our clinic complaining of persistent dizziness that had been affecting her for months. She described it as a “floating” sensation rather than true spinning vertigo. It was worse after long hours at her desk and when she turned her head too quickly. She had seen a GP and undergone tests, but everything came back clear.
Assessment and Diagnosis
After a thorough assessment, we identified that Sarah’s symptoms were cervicogenic in nature—meaning it stemmed from her neck. She had significant muscle tightness in her upper neck, poor posture from long hours at her desk, and limited neck movement.
Physiotherapy Treatment
Sarah’s treatment plan included:
- Manual therapy: Hands-on techniques to release tight neck muscles and improve joint mobility.
- Postural correction: Exercises to strengthen her postural muscles and reduce strain on her neck.
- Balance retraining: Specific exercises to improve her stability and reduce her dizziness episodes.
- Education: Advice on workplace ergonomics and strategies to prevent recurrence.
Outcome
After four weeks of physiotherapy, Sarah reported a significant reduction in her dizziness. She felt more stable, her neck was moving more freely, and she could work without constant discomfort. With ongoing exercises, she was able to return to normal activities without the symptoms interfering in her life.
How to Know if Physiotherapy Can Help
If you experience dizziness, a physiotherapy assessment can help determine the cause. Physiotherapists use specific tests to differentiate between vestibular, neck-related, or other causes.
You may benefit from physiotherapy if you:
- Have your symptoms triggered by head or neck movements.
- Feel unsteady when walking or changing positions.
- Have a history of neck stiffness, poor posture, or recent injury.
- Experience lingering symptoms after a viral illness or concussion.

Final Thoughts
We know it can be frustrating, but you don’t have to live with it. Physiotherapists are well-equipped to assess and treat various forms of dizziness, from BPPV to cervicogenic dizziness. If you have symptoms described in this blog, a physio appointment could be the first step towards feeling steady and confident again.
References and Further Reading
- Better Health Channel. (n.d.). Dizziness and Vertigo. Retrieved from https://www.betterhealth.vic.gov.au
- Vestibular Disorders Association. (n.d.). Vestibular Rehabilitation Therapy. Retrieved from https://vestibular.org
- Physiopedia. (n.d.). Cervicogenic Dizziness. Retrieved from https://www.physio-pedia.com
- Mayo Clinic. (n.d.). Benign Paroxysmal Positional Vertigo (BPPV). Retrieved from https://www.mayoclinic.org
Book an appointment with XPhysio today on 9806 3077!
Abdominal surgery is no small thing—it takes a toll on your body, your mobility, and even your confidence in movement. Whether it’s an appendectomy, hernia repair, caesarean section, or bowel surgery, getting back to normal isn’t as simple as just waiting it out. This is where physiotherapy comes in.
A good recovery plan can help you regain strength, prevent complications, and get back to doing what you love sooner rather than later. In this guide, we’ll walk you through the role of physiotherapy after abdominal surgery and give you practical tips to help you on your way. We have had many patients walk through the door who had been told by their surgeon that they will be fine in time, but they saw notable improvements with our guidance.
Why Is Physiotherapy Important After Abdominal Surgery?
Abdominal Surgery in the abdominal area can have a range of effects on your body, including:
- Pain and discomfort: Surgical wounds, muscle tension, and internal healing can all cause discomfort.
- Reduced mobility: Simple tasks like getting out of bed, bending down, or even breathing deeply can feel difficult.
- Muscle weakness: The core muscles play a huge role in movement, and surgery can disrupt their function.
- Breathing difficulties: Pain and stiffness can make deep breathing harder, increasing the risk of lung infections.
- Risk of complications: Without proper movement and rehab, there’s a higher chance of issues like blood clots, adhesions, or ongoing weakness.
Physiotherapy aims to restore function, improve mobility, and prevent long-term problems.

The Early Days: Hospital Physiotherapy
Most people see a physiotherapist soon after abdominal surgery while still in hospital. The main focus during this stage is:
- Deep Breathing Exercises – To prevent lung infections and keep the lungs clear.
- Gentle Movements – To reduce stiffness and encourage circulation.
- Safe Mobilisation – Learning how to get in and out of bed, stand up, and walk safely without straining the abdominal area.
A common technique is the log roll method—rolling onto your side first before pushing up into a seated position. This reduces strain on the healing tissues.
What Happens When You Go Home?
Once you’re discharged, the real work begins. Recovery can take weeks to months, depending on the type of abdominal surgery and your overall health. Here’s what to focus on:
1. Gentle Movement and Walking
As soon as you’re able, walking should become a daily habit. It promotes circulation, prevents stiffness, and helps restore confidence in movement. Start with short walks around the house and gradually increase the distance.
2. Core and Pelvic Floor Activation
Your abdominal muscles and pelvic floor may be weakened post-surgery. Simple, controlled exercises help to re-engage these muscles without putting too much strain on the area:
- Pelvic tilts – Lying down, gently tilt your pelvis back and forth to activate the deep core muscles.
- Diaphragmatic breathing – Breathe deeply into your belly, focusing on slow, controlled movements.
- Gentle pelvic floor contractions – Engaging these muscles helps with stability and support.
3. Scar and Tissue Management
Once your incision is healing well (usually after 2-3 weeks), gentle scar massage can help prevent adhesions and improve mobility. Use light circular motions with a non-irritating lotion.

When Can You Return to Exercise?
Returning to exercise depends on the type of surgery and your recovery speed. A rough guide is:
- Weeks 1-2: Focus on light walking, deep breathing, and gentle activation exercises.
- Weeks 3-6: Progress to more structured movement like bodyweight exercises and stretching.
- After 6 weeks: Depending on healing, you may start strength training, low-impact cardio, and core work.
Avoid high-impact activities (like running, heavy lifting, or abdominal crunches) until you get the all-clear from your physiotherapist or surgeon.
A Case Study: Emily’s Recovery From Abdominal Surgery
Emily, a 38-year-old office worker, underwent surgery for an umbilical hernia repair. She was fit before surgery but struggled with pain, stiffness, and the fear of moving incorrectly during recovery.
Her physiotherapy plan included:
- Week 1-2: Gentle breathing exercises, walking inside the house, and learning safe bed mobility.
- Week 3-4: Light core activation work, improving posture, and increasing walking distance.
- Week 5-8: Graduating to bodyweight exercises, light yoga, and scar massage.
Exercise Program for Week 5-8:
At this stage, Emily’s physiotherapist introduced a structured program focusing on rebuilding core strength, stability, and overall mobility. Her program included:
- Pelvic tilts (Emily tends to tilt anteriorly at her hips so we introduced this for awareness, lying down, 10 reps x 2 sets)
- Banded Bridging (gentle glute bridges with hip abduction, 10 reps x 2 sets)
- Standing banded hip flexions (standing against a wall, marching with band around feet, 10 reps per side)
- Wall push-ups (gentle upper body activation, 10 reps x 2 sets)
- Side plank on knees with or without leg lifts (to engage the hips and core, 10 reps per side)
- Gentle standing squats (half-depth, focusing on control, 10 reps x 2 sets)
- Walking for 20-30 minutes daily

This program helped Emily regain her strength safely without putting too much strain on her healing abdominal muscles. By 12 weeks, Emily was back to her pre-surgery fitness routine with modifications. Her recovery was smooth thanks to early rehab and consistent progressions.
Common Mistakes to Avoid
- Ignoring pain – While some discomfort is normal, sharp or increasing pain needs to be checked.
- Rushing into exercise too soon – Overdoing it can lead to complications like hernias or muscle tears.
- Neglecting core and pelvic floor activation – These are crucial for long-term recovery and stability.
- Skipping follow-ups – Seeing a physiotherapist ensures you’re progressing safely.
Final Thoughts
Physiotherapy plays a key role in your recovery after abdominal surgery. The right exercises, movement strategies, and gradual progressions can help you return to normal life feeling stronger and more confident. If you’ve had abdominal surgery, working with a physiotherapist ensures you’re moving safely and preventing long-term issues.Give us a call today if you have any questions 02 9806 3077
References:
- Better Health Channel. (n.d.). “Recovering from surgery.” Retrieved from https://www.betterhealth.vic.gov.au
- Australian Physiotherapy Association. (n.d.). “Physiotherapy and post-surgical care.” Retrieved from https://australian.physio
- The Royal Women’s Hospital. (n.d.). “Caring for your body after abdominal surgery.” Retrieved from https://www.thewomens.org.au
If you’re recovering from surgery and need guidance, book a session with a physiotherapist to ensure a smooth and safe recovery!
Let’s have a chat about carpal tunnel syndrome (CTS), a condition that can cause a fair bit of discomfort in your hand and wrist. Understanding what it is, why it happens, and how we can manage it through physiotherapy can make a world of difference.
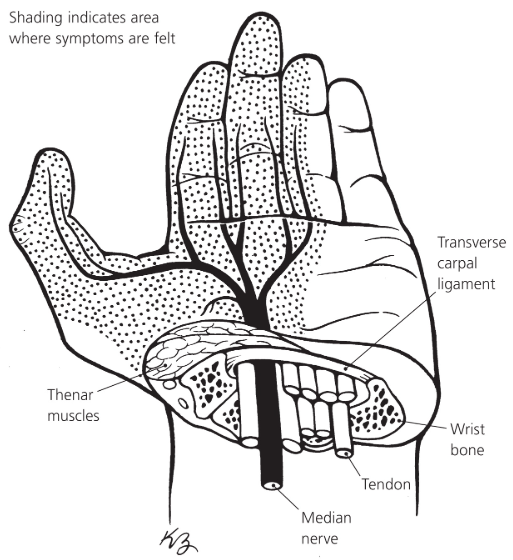
What Is Carpal Tunnel Syndrome?
Imagine a narrow passageway on the palm side of your wrist—about the size of a twenty-cent coin. This is the carpal tunnel, and it houses the median nerve along with tendons that help bend your fingers. When this tunnel becomes cramped or the contents swell, it puts pressure on the median nerve, leading to symptoms like pain, numbness, and weakness in your hand.
Why Does It Happen?
Several factors can contribute to CTS:
- Repetitive Movements: Activities that involve repetitive wrist movements, such as typing or machine work, can increase the risk.
- Wrist Positioning: Keeping your wrist in a bent position for extended periods, like when writing or using a computer mouse, may contribute.
- Health Conditions: Conditions like diabetes, thyroid issues, or arthritis can play a role.
- Pregnancy: Hormonal changes and fluid retention during pregnancy can lead to swelling in the carpal tunnel.
- Anatomy: Some folks naturally have a smaller carpal tunnel, making them more susceptible.
What Are the Symptoms?
CTS often starts with a gradual onset of symptoms, including:
- Numbness or Tingling: Especially in the thumb, index, middle, and ring fingers.
- Pain: In the wrist, palm, or forearm.
- Weakness: You might find yourself dropping objects or having trouble with tasks that require fine motor skills.
- Night-Time Discomfort: Symptoms can be worse at night, sometimes waking you from sleep.
How Can Physiotherapy Help?
Physiotherapy offers a range of treatments to alleviate the symptoms of CTS and improve hand function:
- Education: Understanding the condition and how to manage it is crucial. Your physio can provide guidance on modifying activities to reduce strain on your wrist.
- Splinting: Wearing a wrist splint, especially at night, can keep your wrist in a neutral position, reducing pressure on the median nerve.
- Exercises: Specific exercises can help improve flexibility and strength in the wrist and hand. Here are some exercises that might be beneficial:
Median Nerve Gliding Exercises
These exercises help the median nerve move more freely through the carpal tunnel, reducing pressure and improving symptoms.
Wrist Flexor Stretch
This stretch targets the muscles on the underside of your forearm, helping to relieve tension that may contribute to CTS symptoms.

Wrist Extensor Stretch
Stretching the muscles on the top side of your forearm can also be beneficial in managing CTS discomfort.

Tendon Gliding Exercises
These exercises promote the smooth movement of tendons through the carpal tunnel, reducing stiffness and improving function.

Grip Strengthening Exercises
Strengthening the muscles of the hand can improve overall function and help alleviate symptoms of CTS.

- Manual Therapy: Techniques like gentle mobilization of the wrist joints and soft tissue massage can reduce pain and improve mobility.
- Ergonomic Advice: Your physio can assess your work or home setup and suggest modifications to reduce strain on your wrist.
What Can You Do at Home?
In addition to physiotherapy, there are steps you can take to manage CTS:
- Activity Modification: Take regular breaks from repetitive tasks and avoid positions that overextend your wrist.
- Stretching: Incorporate gentle wrist and hand stretches into your daily routine.
- Ice Therapy: Applying ice to the wrist can help reduce inflammation and alleviate pain.
- Maintain a Healthy Lifestyle: Managing underlying health conditions and maintaining a healthy weight can reduce your risk.
When Should You Consider Surgery?
If symptoms persist despite conservative treatments, or if there’s significant nerve compression, surgical options may be considered. Surgery involves releasing the ligament that’s pressing on the median nerve to create more space in the carpal tunnel. However, many people find relief through physiotherapy and other non-surgical interventions.
Final Thoughts
Carpal tunnel syndrome can be a real nuisance, but with the right approach, you can manage the symptoms effectively. Physiotherapy offers a range of treatments tailored to your needs, aiming to reduce pain, improve function, and enhance your quality of life. If you’re experiencing symptoms of CTS, it’s a good idea to consult with a healthcare professional or physiotherapist to develop a treatment plan that’s right for you.
Remember, early intervention can prevent symptoms from worsening, so don’t hesitate to seek help if you’re experiencing discomfort in your hand or wrist.
Sources
1) Hingehealth
Physical Therapy for Carpal Tunnel: Tips & Best Exercises
Learn how physical therapy for carpal tunnel syndrome can help you manage symptoms and prevent future pain flares through targeted exercises.
2) Choose PT
Physical Therapy Guide to Carpal Tunnel Syndrome – Choose PT
Carpal tunnel syndrome is a common condition that causes pain, numbness, and weakness in the wrist and hand. CTS can affect the use of the entire arm.
3) Physiopedia
Carpal Tunnel Syndrome – Physiopedia
Carpal tunnel syndrome (CTS) is an entrapment neuropathy caused by compression of the median nerve as it travels through the wrist’s carpal tunnel.
4) ASSH
What is Carpal Tunnel Syndrome? | The Hand Society
5) Australian Sports Physiotherapy
Carpal Tunnel Syndrome Physio – Australian Sports Physiotherapy
Most carpal tunnel syndrome patients benefit from physiotherapy, particularly those with mild to moderate symptoms.
Carpal Tunnel Syndrome – Exercise Thought
Carpal Tunnel Syndrome (CTS) is a condition of the hand where the median nerve becomes compressed
When most of us think of physiotherapists, we often picture them helping people with sports injuries, sore backs, or post-surgery rehabilitation. But did you know that physiotherapists can also help treat headaches? Yep, you heard that right. If headaches are making your life miserable, seeing a physio might be a game-changer. Let’s dive into the types of headaches they can treat and how they work their magic to help you feel like yourself again.
Understanding Headaches: A Quick Overview
Before we get into the nitty-gritty, it’s worth knowing that not all headaches are the same. Different types have different causes, and that’s why the treatment varies. While some require medical intervention or medication, others can stem from physical issues that a physio can address. Things like poor posture, muscle tension, or even stress can trigger them that are within a physio’s expertise to manage.
Now, let’s look at the types of headaches physiotherapy can help with.
1. Tension Headaches
Tension headaches are incredibly common, and chances are you’ve experienced one at some point. They feel like a tight band squeezing around your head or a dull, aching pressure. Often, they will result from stress, poor posture, or prolonged time in one position (hello, desk workers!).
How can a physio help?
- Postural Corrections: Your physio w ill assess your posture and help you make adjustments to reduce strain on your neck and shoulders.
- Massage Therapy: Tense muscles, particularly in the neck, shoulders, and upper back, are often the culprits. Massage can work wonders to release that built-up tension.
- Exercise Programs: Simple exercises can strengthen your muscles, improve flexibility, and prevent future headaches.
2. Cervicogenic Headaches
Cervicogenic headaches are a mouthful to say, but they’re fairly straightforward in how they occur. They will often start in the neck but are felt in the head, and typically only on one side. They’re typically caused by joint or muscle issues in the neck, poor posture, or even an injury like whiplash.

How can a physio help?
- Manual Therapy: Techniques like joint mobilisation or manipulation can help restore proper movement and reduce pain.
- Dry Needling: This technique involves inserting thin needles into trigger points in your muscles to relieve pain and tension.
- Neck Strengthening Exercises: Weak neck muscles can contribute to cervicogenic headaches, so your physio may give you targeted exercises to build strength.

3. Migraines
Migraines are a bit more complex. They’re often accompanied by nausea, sensitivity to light or sound, and a throbbing pain that can last for hours or even days. While migraines are usually managed with medication, physiotherapy can play a supportive role, especially if physical triggers are contributing to them.
How can a physio help?
- Identifying Triggers: Your physio can help you identify physical triggers like tension or poor posture that may be setting off your migraines.
- Relaxation Techniques: Stress and tension can exacerbate migraines, so learning how to relax your muscles can be incredibly helpful.
- Improving Sleep Posture: How you sleep matters. Your physio might recommend changes to your sleep setup to reduce strain on your neck.
4. Cluster Headaches
Cluster headaches are less common but incredibly intense. They’re often described as a piercing or burning pain around one eye and typically occur in clusters (hence the name) over weeks or months. While physios can’t treat the root cause of the cluster type, they can help manage some of the secondary symptoms.
How can a physio help?
- Pain Management Strategies: Techniques like gentle massage and relaxation exercises can help reduce overall tension and discomfort.
- Improving Overall Wellbeing: Your physio might focus on general health and stress management to support your body during these episodes.
5. TMJ-Related Headaches
Your temporomandibular joint (TMJ) connects your jaw to your skull, and issues with this joint can lead to headaches. TMJ-related pain is often felt in the jaw with clicking or popping sounds, and even difficulty opening or closing your mouth.
How can a physio help?
- Jaw Exercises: Specific exercises can improve the function of your TMJ and reduce pain.
- Massage and Stretching: Releasing tension in the jaw and surrounding muscles can work wonders.
- Postural Adjustments: Since your jaw and neck are closely linked, improving your posture can alleviate symptoms.

6. Headaches Following a Concussion
If you’ve had a concussion, headaches can linger long after the initial injury. These are often due to neck issues, muscle tension, or even changes in how you move as your body compensates for the injury.
How can a physio help?
- Neck Rehabilitation: Addressing any stiffness or weakness in your neck can help reduce the pain.
- Balance and Coordination Exercises: If your concussion has affected your balance, your physio can guide you through exercises to restore it.
- Education: Your physio can teach you strategies to pace yourself during recovery and avoid activities that might aggravate your symptoms.
How to Know If Your Headache Is Physio-Treatable
Not every headache will benefit from physiotherapy. If it is sudden, severe, or accompanied by symptoms like vision changes, confusion, or weakness, you should seek medical attention immediately. But if it seems tied to physical tension, mental stress, posture, or previous injuries, a physio might be just what you need.
Signs your physio might be able to help:
- You notice stiffness or discomfort in your neck, shoulders, or jaw.
- Your pain comes on after sitting for long periods.
- You’ve had a recent injury or accident.
- Stress or tension seems to make things worse.
What to Expect During a Physio Appointment
If you’ve never been to a physio for headaches before, you might be wondering what’s involved. Here’s a quick rundown:
- Assessment: Your physio will ask about your pain history, lifestyle, and any other symptoms you’re experiencing. They’ll also assess your posture, muscle tension, and joint movement.
- Treatment Plan: Based on their findings, your physio will create a tailored treatment plan. This might include manual therapy, strengthening exercises, or advice on ergonomics.
- Hands-On Treatment: Techniques like massage, mobilisation, or dry needling may be used to address tension and pain.
- Home Exercises: Your physio will likely give you some exercises to do at home to support your recovery and prevent future pain.

Tips for Preventing Headaches
Prevention is always better than cure, right? Here are some tips to keep headaches at bay:
- Move Regularly: If you sit for long periods, take breaks to stretch and move around.
- Check Your Posture: Make sure your desk setup is ergonomic and that you’re not slouching.
- Manage Stress: Find ways to relax, whether it’s through yoga, meditation, or a walk in the park.
- Sleep Well: A good night’s sleep can do wonders for headache prevention. Pay attention to your pillow and sleeping position.
Wrapping It Up
Headaches can be a real pain—literally—but they don’t have to take over your life. Physiotherapy offers a range of treatments that can help alleviate the pain and prevent it from coming back. Whether it’s tension headaches, cervicogenic headaches, or even migraines, a physio can help you tackle the root cause and get back to feeling your best.
So, if headaches are getting you down, why not book an appointment with a physiotherapist at XPhysio today? You’ve got nothing to lose—except the headache, of course!
