As we age, it’s no secret that our bodies go through all sorts of changes. Most of these changes are completely normal, but when it comes to our muscles, joints, and bones, it’s easy to feel concerned—especially when you get a scan that highlights degenerative changes. The medical terminology on these scans can feel overwhelming, and often, the results don’t differentiate between normal, age-related changes and the possible causes of symptoms. This can lead to a lot of confusion and stress. It’s not uncommon for people to misinterpret their scan results, believing they are in worse condition than they actually are.
In this blog, we’re going to break down some common age-related degenerative changes, how to understand your scan results, and highlight the importance of working with a physiotherapist to properly interpret them. Plus, we’ll touch on some incidental findings—things that show up on scans but may not be as concerning as they sound.
The Complexity of Pain and Scans
Before we dive into the specifics, it’s important to understand that pain is a complex process. It’s our body’s natural defence mechanism, designed to protect us from harm. But here’s the tricky part: damage doesn’t always cause pain, and just because you feel pain, it doesn’t mean there’s necessarily damage.
Thanks to ongoing research, we now know that scans don’t always paint the full picture when it comes to pain. Studies comparing the scans of people with and without symptoms have revealed that many people walk around with some form of “damage” or pathology on their scans, but they experience no pain at all. In fact, many of these individuals go about their daily lives without any issues. This is where things can get confusing—just because something shows up on a scan doesn’t mean it’s causing your pain or needs to be treated.
Age-Appropriate Degenerative Changes: What’s Normal?
As we age, there are a few changes that naturally occur in our musculoskeletal system. These changes might sound scary when you see them listed on a scan, but the reality is that they’re a normal part of the aging process. Here’s a look at some common age-appropriate degenerative changes:
1. Joint Health
As we get older, the cartilage that cushions our joints naturally starts to wear down. This can lead to conditions like osteoarthritis, where the joints become stiff and painful. However, just because you see signs of wear and tear in a joint on your scan doesn’t mean you’ll experience symptoms. Many people have signs of joint degeneration on their scans but experience little to no discomfort.
2. Bone Density
Our bones naturally lose density as we age, which makes them more susceptible to fractures. This is why conditions like osteoporosis become more common in older adults. Decreased bone density can show up on a scan, but it’s something that can often be managed with diet, exercise, and, in some cases, medication.
3. Muscle Mass and Strength
As we age, we also lose muscle mass and strength—a condition known as sarcopenia. This loss of muscle can impact mobility and increase the risk of falls, but it’s a gradual process that can often be slowed or reversed with regular strength training and physiotherapy.
4. Posture and Alignment
Changes in our spinal discs and ligaments are a common part of aging, and these changes can sometimes lead to alterations in posture or spinal alignment. For example, you might develop a slight hunch or notice that your range of motion isn’t what it used to be. While these changes are normal, they can sometimes contribute to discomfort, which is why maintaining flexibility and mobility through exercise is key.
5. Flexibility and Range of Motion
As we get older, our connective tissues, like tendons and ligaments, become less flexible. This can lead to a gradual reduction in range of motion, which is why it’s so important to stay active and keep those muscles and joints moving.

Incidental Findings on Scans: What Do They Mean?
Now that we’ve covered some common degenerative changes, let’s talk about incidental findings—those things that show up on your scan that might sound alarming but are often completely normal. Here are a few examples based on common areas of the body:
1. Shoulder
A study conducted in 2013 looked at the prevalence of full-thickness rotator cuff tears across different age groups. They found that:
- 0% of people in their 20s to 40s had full-thickness tears.
- 10% of people in their 50s had full-thickness tears.
- 15% of people in their 60s had full-thickness tears.
- 36% of people in their 80s had full-thickness tears.
Interestingly, 65% of the people with rotator cuff tears didn’t experience any symptoms. That means that a significant number of people were walking around with these tears but were pain-free and functioning normally. If something like this shows up on your scan, it doesn’t necessarily mean it’s causing your pain or needs surgical intervention.

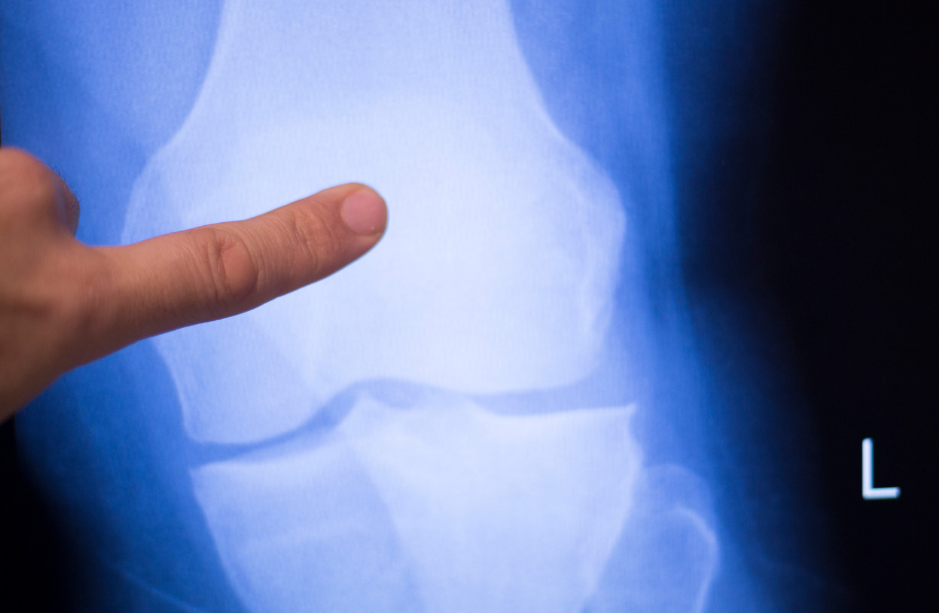
2. Knee
A study focused on individuals aged 50 to 90 looked at the prevalence of meniscal tears in this age group. The results showed:
- 19% of females aged 50-60 had meniscal tears.
- 56% of males aged 70-90 had meniscal tears.
What’s surprising is that only 61% of these individuals reported experiencing knee pain in the past month. This highlights that, while meniscal tears are common as we age, they aren’t always associated with symptoms.
3. Back
There’s been a lot of research done on back pain and how it correlates (or doesn’t) with scan results. A recent study showed that:
- 37% of pain-free 20-year-olds had evidence of disc degeneration on their scans.
- A whopping 96% of pain-free 80-year-olds had disc degeneration.
Again, this shows that degenerative changes in the spine are common as we age and don’t always result in pain. If your scan comes back showing disc degeneration, it’s important to remember that it’s a normal part of aging and may not be the root cause of any discomfort you’re experiencing.
Why You Are Not Your Scan
Here’s the takeaway: you are not your scan. Medical imaging is incredibly useful for diagnosing certain conditions, but it has its limits. Scans can pick up every little detail—things that may have been there for years without causing any issues. Just because something abnormal shows up doesn’t mean it’s causing your pain or needs treatment.
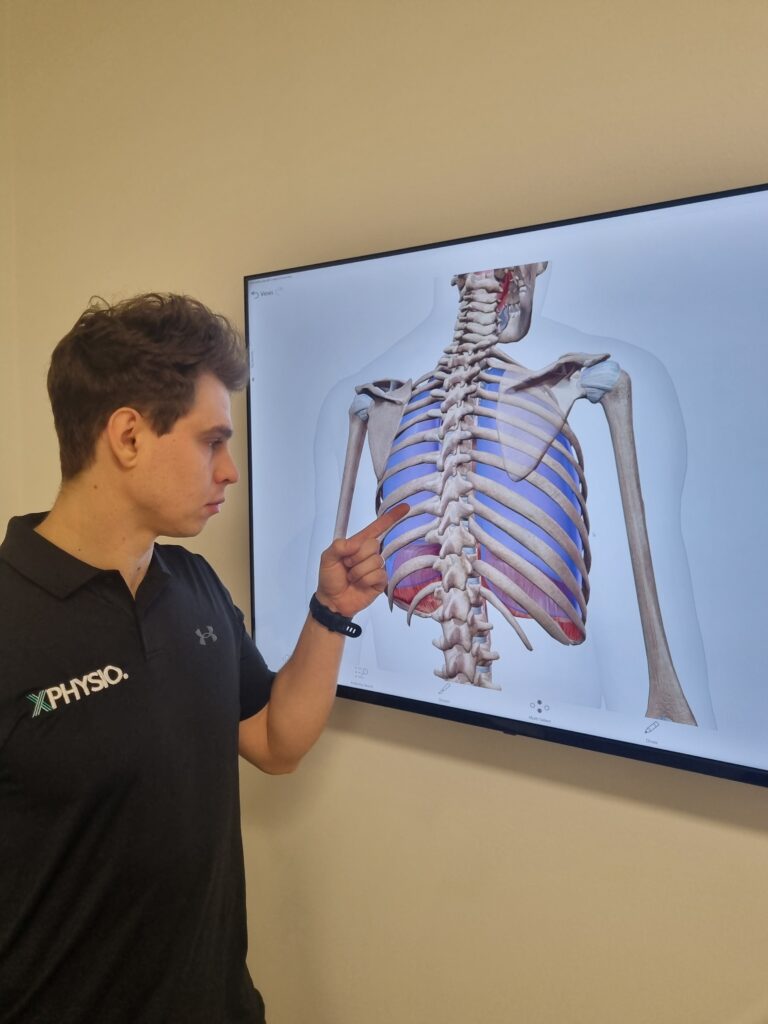
That’s why it’s so important to consult with a physiotherapist who can assess your symptoms, examine your scan results, and give you a comprehensive, real-world interpretation. A physio will be able to help you understand which findings on your scan are normal for your age and which ones might be contributing to your symptoms. They’ll also guide you through a treatment plan that’s focused on getting you back to feeling your best, without unnecessary worry about incidental findings.
Physiotherapy for Age-Appropriate Degenerative Changes
Physiotherapy is one of the best ways to manage age-related changes in your musculoskeletal system. Here are some of the interventions that a physiotherapist might use to help you stay active and healthy as you age:
1. Exercise Prescription
Staying active is one of the most effective ways to manage degenerative changes and maintain your overall health. A physiotherapist can design a tailored exercise program that includes strength training, flexibility exercises, and cardiovascular activities. This type of program will help you build muscle, maintain joint health, and improve your balance and coordination.
2. Pain Management Techniques
If you’re experiencing pain related to degenerative changes, a physiotherapist can use a variety of techniques to help manage it. These might include manual therapy (such as massage or joint mobilisation), heat and cold therapy, and even dry needling. The goal is to reduce pain while improving your overall function.
3. Balance and Fall Prevention
As we age, our risk of falls increases, particularly if we’ve lost muscle strength or balance. Physiotherapists can guide you through balance exercises and functional training to improve your stability and reduce your risk of falling. This is especially important for older adults, as falls can lead to serious injuries like fractures.
4. Joint Mobilisation and Soft Tissue Techniques
If joint stiffness or muscle tightness is limiting your range of motion, physiotherapists can use hands-on techniques to help. Joint mobilisation can improve the movement of stiff joints, while soft tissue techniques can address tight muscles and help you move more freely.
Conclusion
Aging is a natural process, and age-appropriate degenerative changes are nothing to fear. In fact, understanding these changes is the first step toward maintaining a healthy, active lifestyle well into your later years. Physiotherapy plays a crucial role in this journey, offering targeted interventions that can help you manage pain, maintain mobility, and stay strong.
Remember, the next time you get a scan back, don’t be alarmed by every detail. Work with one of our physiotherapists at XPhysio who can help you interpret the results and provide a clear path forward. By staying proactive and taking care of your body, you can enjoy a fulfilling, active life, no matter your age!
You could have sworn someone had just kicked you from behind as you fell onto your knees, immediately losing all power in your leg. But when you turned around, there wasn’t anyone in sight. A sharp pain shoots through your leg, and you reach down to feel a strange divot at the back of your ankle. That’s when it hits you—something’s gone seriously wrong. You’re already thinking, “This is going to need surgery, no question.”
But here’s the thing—you might be wrong!
Believe it or not, Achilles ruptures are now often treated without surgery, using early immobilisation instead. Recent studies have shown that there’s only a minimal difference in the re-rupture rates between patients who go the surgical route and those who opt for conservative management. It’s a pretty big shift in how this injury is treated, and if your specialist agrees that your case is suitable for non-surgical treatment, it could mean avoiding the risks and recovery time associated with surgery altogether. Not bad for an injury that many people assume automatically requires going under the knife!

Understanding Achilles Rupture
Before we get into the nitty-gritty of treatment, it’s worth understanding a bit more about what an Achilles rupture actually is and how it happens.
Anatomy of the Achilles Tendon
The Achilles tendon is the largest and strongest tendon in the human body. It connects the calf muscles—specifically the gastrocnemius and soleus—to the heel bone (the calcaneus). This tendon plays a key role in everyday movements like walking, running, jumping, and even standing on your toes. Anytime you push off the ground with your foot, you’re engaging your Achilles tendon.
Because the Achilles tendon handles so much load and repetitive stress, it’s particularly vulnerable to injury. Ruptures occur when the tendon is suddenly overloaded, and the force is too great for the tissue to handle.
Cause
There are a few common scenarios where an Achilles rupture is likely to occur:
Sudden Forceful movements: This is often the culprit in ruptures, particularly during activities that involve a rapid change in direction or explosive pushing off. Think sports like basketball, football, tennis, or sprinting, where you need to go from stationary to full speed in a split second.
Chronic overuse: Over time, repetitive stress can weaken the Achilles tendon. This is especially common in athletes who don’t give their body enough time to recover between intense training sessions, or people who do a lot of walking or running on hard surfaces. Overuse creates micro-tears in the tendon, and over time, this wear and tear can lead to a full rupture.
Age and activity level: ruptures are more common in people aged 30 to 50, particularly those who engage in “weekend warrior” activities—high-intensity sports without proper conditioning or preparation. Tendons naturally become less elastic and more prone to injury as we age.

Symptoms of Achilles Rupture
Achilles ruptures are typically dramatic, and the symptoms aren’t hard to miss:
Sharp Pain: People often describe the pain of an Achilles rupture as feeling like they’ve been kicked or hit in the back of the leg. Some even hear a “pop” or “snap” when the tendon gives way.
Divot at the back of the ankle: If you feel a noticeable gap or divot where the Achilles tendon should be, that’s a classic sign of rupture.
Swelling and tenderness: The back of the leg and ankle will swell up fairly quickly after the injury, and the area will likely be very tender to the touch.
Difficulty walking: A ruptured Achilles tendon makes it extremely hard to push off your foot, making walking difficult. You may have a limp or find it impossible to bear weight on the injured leg.
Physiotherapy Interventions
If you’ve just experienced a rupture, you’re probably wondering what the next steps are. This is where a physiotherapist can make all the difference. Whether you end up going the surgical or non-surgical route, a tailored rehabilitation plan is crucial to ensure proper healing and to minimise the risk of re-injury.
Non-Surgical Management
More and more often, non-surgical management is being recommended for ruptures, especially for people who aren’t high-level athletes. The idea is that by immobilising the ankle and gradually increasing the range of motion and load through the tendon, the body can heal itself.
At XPHYSIO, we collaborate closely with a number of trusted orthopaedic surgeons. If you’ve been diagnosed with an Achilles rupture, we can arrange for you to be seen by a specialist who will help determine whether surgery is necessary or if non-surgical management is the better option. If non-surgical treatment is chosen, we would fit you with a VACOped CAM boot or a similar walker. These boots are designed to keep your foot at the right angle for optimal healing while allowing for adjustments over time as the tendon repairs itself.

Tip: These timelines are averages. Your progress may be faster or slower depending on your age, fitness, and the severity of the rupture. A physiotherapist will adjust your plan based on how your tendon responds.
Post-Surgery Rehabilitation
If surgery is necessary, rehabilitation becomes even more important. A physiotherapist will guide you through the post-surgical recovery process, ensuring that the tendon heals properly and regains its strength and flexibility.
Some key elements of post-surgery rehabilitation include:
Range of motion exercises: After surgery, the ankle is often stiff, and you’ll need to do gentle range-of-motion exercises to restore flexibility without putting too much stress on the healing tendon.
Strengthening Protocols: As you progress in your recovery, strengthening the muscles of the calf and the Achilles tendon is crucial. A physiotherapist will guide you through a gradual progression of exercises designed to rebuild strength without overloading the tendon too early.
Gait Training: After an Achilles rupture, walking normally can feel like a distant goal. A physiotherapist will work with you to retrain your gait and restore a natural stride, reducing the likelihood of compensatory movements that could lead to further injury.
Functional Exercises: These are exercises that mimic the movements you’ll be doing in your day-to-day life or sports activities. For example, if you’re a runner, your physiotherapist will incorporate exercises that prepare your Achilles tendon for the specific stresses of running.
Gradual Progression: The key to successful rehabilitation is a phased approach. Your physiotherapist will create a program that gradually increases the intensity and load on your Achilles tendon, ensuring that you don’t do too much too soon and risk a re-rupture.
To learn more about post surgery rehab, read out blog HERE
Typical Recovery Timeline For Both Conservative or Surgical
Whether you’re managed conservatively or after surgery, the broad principles of rehab are very similar. At XPHYSIO we individualise every program, but here’s what a standard evidence-based timeline often looks like:
- 0–4 Weeks: Non-Weight Bearing
In the first few weeks the goal is protection. The ankle is held in plantarflexion (toes pointed down) in a boot or cast to take stress off the healing tendon. You’ll usually be on crutches and non-weight bearing, although gentle toe wiggling and circulation exercises may be encouraged. - From 4 Weeks: Begin Partial Weight Bearing (up to 50%)
Once the tendon has begun to knit together, you can start carefully loading it. Most people move to partial weight bearing in the boot at about 4 weeks, using crutches for balance. This introduces controlled stress that stimulates the tendon to heal stronger. - 5–6 Weeks: Gradual Reduction of Plantarflexion
The boot angle is reduced by around 5 degrees every five days (or as instructed by your specialist). This slowly brings the foot closer to a neutral position, allowing the tendon to adapt to length changes without being overstretched. - By 9 Weeks: Achieving Full Plantar Grade
Around the 9-week mark, most people reach neutral (plantar grade) in their boot. This means the ankle is in a normal standing position and the tendon is tolerating a functional length. - 6–12 Weeks: Restoring Range of Motion
During this phase, gentle, supervised ankle mobility exercises are introduced. The aim is to restore normal dorsiflexion (bringing the foot upwards) and plantarflexion while respecting the healing tissue. - 12–20 Weeks: Strengthening Phase
As movement normalises, more active strengthening of the calf muscles begins—initially seated or isometric exercises, progressing to standing heel raises, balance work, and light functional drills. - 5–7 Months: Return to General Activity
Everyday activities like brisk walking, cycling, or gym work can usually be resumed gradually. Plyometric or high-impact exercise is still limited at this point however we are building your capacity for your chosen sport. - 8–12 Months: Return to Play/Sport
This is the period where advanced sport-specific conditioning occurs—running drills, cutting, jumping, sprinting. Return-to-play testing ensures your tendon strength and function are symmetrical and your risk of re-rupture is low.
Preventive Measures
Once you’ve fully recovered from an Achilles rupture, it’s important to take steps to prevent the injury from happening again. The Achilles tendon will be stronger, but it’s still vulnerable, particularly in the first year after injury. Here are some tips to keep your Achilles tendon healthy:
Proper Warm-up and Cool Down
This is something many of us skip, but it’s especially important after an Achilles rupture. Warming up properly increases blood flow to the muscles and tendons, making them more elastic and ready for exercise. Cooling down helps flush out lactic acid and promotes recovery. At XPHYSIO, we can provide you with a tailored warm-up and cool-down routine that suits your activity level.
Footwear and Equipment
Wearing the right shoes is another important preventive measure. Look for footwear that provides proper support for the arch of your foot and has good cushioning to reduce impact. If you’re an athlete, make sure your equipment (e.g. orthotics) is up to scratch and not worn out.
Cross-Training
Avoid doing the same type of exercise over and over, as this can lead to overuse injuries like an Achilles rupture. Instead, mix it up! Incorporate a variety of activities into your routine—swimming, cycling, yoga, strength training—to reduce stress on the Achilles tendon and work different muscle groups.
Conclusion
An Achilles rupture can feel like a devastating setback, especially if you’re active or involved in sports. But the good news is that with the right treatment, full recovery is achievable. Whether you go down the surgical or non-surgical route, working with a physiotherapist to create a personalised rehabilitation plan is critical to getting back on your feet—lit erally and figuratively.
At XPHYSIO, our team is here to help you through every step of your recovery. From initial diagnosis to rehabilitation and preventive care, we provide the support and expertise you need to make a successful comeback. With patience, dedication, and the right guidance, you’ll not only recover but come back stronger and more resilient than before.
So, if you’ve recently ruptured your Achilles or you’re experiencing symptoms that have you worried, don’t wait—reach out to a physiotherapist today and start your journey to recovery. You’ve got this!
References
Ochen Y, Beks RB, van Heijl M, Hietbrink F, Leenen LPH, van der Velde D, Heng M, van der Meijden O, Groenwold RHH, Houwert RM (2019). Operative treatment versus nonoperative treatment of Achilles tendon ruptures: Systematic review and meta-analysis. BMJ. 2019 364: 5120.
