Growing pains are common, usually affecting children aged 3-16, causing aching or throbbing in the legs—especially in the thighs, calves or behind the knees—often in the evening or at night. Paediatric physiotherapy offers relief through assessment, stretches, strengthening, and biomechanics education. Read on to discover tips, real clinic outcomes, and what to watch for.
What Are Growing Pains?
“Growing pains” (sometimes called recurrent limb pains of childhood) are benign and relatively frequent in kids. While the name suggests growth is the culprit, there’s no solid evidence that growth itself causes damage. More likely, a combination of muscle fatigue, biomechanical factors, and activity levels contributes. (Health Times+3Sydney Physio Clinic+3Nelson Bay Physiotherapy+3)
Common features:
- Usually affects both legs, not just one. – Canberra Children’s Physiotherapy+1
- Pain tends to occur in muscles (thighs, calves), not in joints. – Nelson Bay Physiotherapy+2Sydney Physio Clinic+2
- Occurring in the late afternoon or evening; often wakes the child at night. – Health Times+2Sydney Physio Clinic+2
- No obvious swelling, redness or signs of infection. – Sydney Physio Clinic+1
- Typically, children still play, walk and run during the day; pain does not usually limit daytime activity. – Nelson Bay Physiotherapy+1

Why Paediatric Physiotherapy?
Paediatric physiotherapy is a specialised branch focused on children’s developmental, skeletal, and muscular needs. Because kids aren’t just “small adults,” treatments must be tailored to their growth phases, movement patterns, muscle strength, flexibility, coordination, and habits.
Physiotherapists can:
- Perform a thorough assessment to rule out other causes (e.g. conditions like Osgood-Schlatter, Sever’s disease, Sinding Larsen Johansson Syndrome, Other Apophysitis’, or joint issues). – Learn more about OSGOOD-SCHLATTERS
- Analyse biomechanics: foot posture, alignment (knock knees, flat feet), muscle tightness or weakness.
- Design stretching programs to ease muscle tightness, especially before bed.
- Introduce strengthening exercises to support joints and reduce strain.
- Provide manual therapy (massage, soft tissue work), heat/cold options, and sometimes use modalities depending on what’s safe.
- Educate parents & kids on activity modification, rest, good footwear, habits like stretching after activity.

Practical Strategies You Can Try at Home
While physiotherapy is super helpful, there are several things parents can try at home in between sessions:
- Warm baths or heat packs in the evening to relax tight muscles.
- Gentle massage of sore muscles.
- Stretching routines for calves, hamstrings, thighs—especially after active play.
- Ensure rest periods after high activity days; avoid over-loading.
- Proper footwear that supports arches; avoid too-flat or too-unsupportive shoes.
- Maintain a consistent sleep routine; fatigue can worsen perception of pain.
- If needed, simple analgesics like paracetamol (always follow dosage guidelines or medical advice).
When to See a Physiotherapist or Other Health Professional
Growing pains are usually harmless, but there are warning signs that mean you shouldn’t just wait it out. Seek professional advice and specifically paediatric physiotherapy if your child:
- Has pain in only one leg or joint, or if it’s localised, swollen, warm, red.
- Is limping, or pain severely limits walking or running.
- Has fever, general illness, weight loss or other systemic symptoms.
- Pain persists steadily beyond the age when growing pains normally fade (often mid-adolescence). Australian Sports Physiotherapy+1
A physiotherapist can both screen for serious issues and guide effective management.

Real-Life Example: Improvement in the Clinic
Here’s a case we saw recently at our clinic in Frenchs Forest, NSW:
Patient: “Sam”, age 8, from a surrounding suburb (in Davidson).
Presentation: Complained of aching calves and thighs in both legs, mostly at night, for about 6-8 weeks. Sleep was disturbed. No limping, no swelling or redness. Very active during the day (lots of jumping, sport).
Paediatric Physiotherapy Assessment : Identified tight calf muscles, slight flat feet, some postural imbalances (leaning forward when standing).
Treatment plan:
- Twice-weekly sessions for 4 weeks: manual soft tissue massage, focused calf & hamstring stretches, core and hip stabilisation strengthening exercises.
- Home program: stretching before bed, with parent-assisted gentle massage, using a warm bath; advice on better footwear.
- Education to both Sam and his parents about when pain is typical vs when to rest or modify activity.
Outcome: After 4 weeks, the nighttime pains reduced significantly: Sam slept through the night most days, pain episodes dropped from nightly to occasional. By 8 weeks, Sam reported almost no pain, was back to full participation in sport, and was happier (and parents were more relaxed).
Additional Benefits Beyond Pain Relief
Paediatric physiotherapy doesn’t just help with immediate discomfort. Longer-term gains include:
- Better motor skills and coordination.
- Improved posture and running/walking mechanics.
- Reduced risk of overuse injuries.
- More confidence in movement and play.

Myths & Misconceptions
| Myth | Reality |
|---|---|
| Growing pains are caused by growing bones rubbing together. | Bones themselves aren’t “pain sensors” like that. Other structures (muscles, tissues) are more likely involved. |
| If a child is active, more sport will resolve it naturally. | Activity helps—but too much without recovery, or poor biomechanics, may increase discomfort. A balance is needed. |
| Pain = damage. | Not in most growing pains. They aren’t signs of harm when diagnosed properly. |
How Long Do Growing Pains Last?
It varies. Many children outgrow them by around age 12-14, though some have symptoms earlier and others later. The frequency/intensity tends to reduce over time, especially with appropriate support and management.
Role of Paediatric Physiotherapy in Preventing Recurrence
Because recurrence is typical, prevention is key:
- Regular stretching and strength maintenance.
- Checking footwear, changing it if it’s worn.
- Encouraging balanced play (not just one sport, one kind of movement).
- Ensuring rest and recovery; listening to the child’s pain signals.
- Periodic assessments, especially during growth spurts.
Beyond the Legs – Why Some Kids Get Pain Elsewhere
While growing pains most often strike the legs, some kids also complain of aches in the arms, back or shoulders after busy days. This doesn’t always mean something is wrong. Children are constantly experimenting with new sports, climbing, running and jumping, which puts extra stress on developing muscles and joints. Paediatric physiotherapy looks at the whole body, not just the sore spot, so underlying imbalances are picked up early and addressed before they cause ongoing pain or poor movement patterns.
The Emotional Side of Growing Pains
Night-time pain can disrupt sleep for both kids and parents, and tired kids may become anxious or less confident in sport. A big part of our role in paediatric physiotherapy is reassurance and education. We explain to children (in age-friendly language) what’s happening in their bodies and give them simple ways to self-manage discomfort. This builds resilience and helps them feel in control rather than fearful of the pain.
Collaboration with Other Health Professionals
Sometimes your physio may liaise with your GP, podiatrist or paediatrician to make sure nothing else is contributing to the pain. For example, custom foot orthotics or a GP check-up may be suggested if biomechanics or vitamin deficiencies are suspected. This team-based approach ensures your child gets the right care at the right time and nothing important is missed, which is one of the strengths of working with a clinic experienced in paediatric physiotherapy.
Setting Kids Up for a Lifetime of Healthy Movement
The habits kids learn now last well into adulthood. Teaching proper stretching, warm-ups, and posture during growth spurts lays the foundation for injury prevention and sporting success later on. Many parents who bring their children to us for growing pains are surprised at how much more confident and coordinated their kids become in sport and everyday play after a few weeks of tailored paediatric physiotherapy.
Summary: What You Can Do Next
- Don’t ignore recurring nighttime leg or muscle aches.
- Book an assessment with a physiotherapist who has experience in paediatric physiotherapy.
- Use home strategies alongside clinic-led treatment.
- Watch for red flags and act promptly.
Final Words
If your child is waking up with leg aches, complaining about sore calves or thighs, or just seems uncomfortable at night—all things a lot of parents brush off—don’t wait. Paediatric physiotherapy can make a big difference: relief, rest, and better days ahead. We treat children however we don’t treat all conditions that a child might have. We specialist in musculoskeletal conditions within children. If you aren’t sure if we treat your particular injury or condition, Call our reception team today on 9806 3077
References
- Upside Kids Physio: Growing Pains: Explore Origins, Management, and When to Consult a Paediatric Physiotherapy Expert Upside Kids Physio
- HealthTimes: Physiotherapy for Managing Growing Pains in Australian Pre-Teens Health Times
- Sydney Physio Clinic: Growing Pains in Children Sydney Physio Clinic
- Nelson Bay Physiotherapy: Growing Pains in Children Nelson Bay Physiotherapy
- Queensland Physiotherapy: Relief For Growing Pains in Children & Teens qldphysio.com.au
Arthritis physiotherapy helps reduce pain, stiffness and improves joint movement by using tailored strength, flexibility and mobility work — all without needing surgery or heavy meds. This blog digs into the best exercises, techniques, and real-life wins, plus what you can start doing now to feel better.
What Is Arthritis & Why It Causes Stiffness
Arthritis isn’t a one-size-fits‐all issue. It’s a broad term for over 100 joint conditions — the most common being osteoarthritis (wear and tear) and rheumatoid arthritis (autoimmune-driven inflammation). (Reference: CSP+2Total Health Clinics+2)
Stiffness happens because:
- Cartilage wears down, bones and soft tissue rub.
- Inflammation causes swelling.
- Muscles around the joint get weak due to less movement.
- People avoid using stiff joints, which leads to more stiffness.

The New View on Osteoarthritis
It’s no longer seen as just “wear and tear.” Research now shows osteoarthritis also has a metabolic and inflammatory side. Carrying extra weight, poor diet, smoking and inactivity can drive low-grade inflammation that speeds up cartilage breakdown and slows repair. This means lifestyle changes and physio — strengthening muscles, improving mobility and keeping you active — can directly reduce both joint load and inflammatory stress, giving you better results than exercise or medication alone.
Why Rheumatoid and Other Autoimmune Types Develop
Unlike osteoarthritis, which is mainly mechanical and metabolic, rheumatoid arthritis and other autoimmune types occur when the immune system misfires. Instead of protecting you, it mistakenly attacks the lining of your joints (the synovium), triggering chronic inflammation, swelling and pain. Over time this can damage cartilage, bone and ligaments. The exact cause isn’t fully understood, but a mix of genetics, hormonal changes, infections and environmental triggers (like smoking) can set it off. Early diagnosis, medical care and physiotherapy together can help control symptoms, protect joints and maintain function.

How Arthritis Physiotherapy Helps
Here’s what physio actually does and why it works naturally:
- Personalised Assessment
Physios assess joint range of motion, strength, alignment, daily habits. From there, they build a treatment plan that suits you. Arthritis Foundation+1 - Strength & Muscle Support
Weak muscles mean more load on joints. Strengthening exercises reduce pain and improve stability. Physio Ed.+2The Physio Box+2 - Increasing Flexibility & Mobility
Gentle stretching, joint mobilisation, range of motion work helps ease stiffness and lets you move more freely. Versus+2Physio Ed.+2 - Pain Management Techniques
Using heat or cold packs, massage, manual therapy, TENS (nerve stimulation), possibly aquatic therapy. All good for reducing pain and inflammation. Spectrum Health+3Versus +3Wikipedia+3 - Education & Self-Management
Teaching you things like joint protection, pacing, posture, how to modify daily tasks so you minimise flare-ups. This helps you take control. CSP+2Spectrum Health+2 - Long-Term Maintenance & Prevention
The aim isn’t just “feel better now” — it’s keeping joints as mobile as possible, reducing further damage, improving quality of life. Spectrum Health+1

Techniques & Exercises That Actually Work
Here are tried-and-tested physiotherapy methods to ease stiffness in arthritis:
| Approach | What It Involves / Example | Benefits |
|---|---|---|
| Strength Training | Using resistance bands, body-weight or machines focused around hips, knees, shoulders etc. | Improves joint stability, takes load off sore joints. |
| Range of Motion (ROM) & Stretching | Gentle stretching, yoga‐like movements, weighted or passive motions done regularly. | Keeps joints from locking up, reduces morning stiffness. |
| Low Impact Aerobic Exercise | Swimming, walking, cycling or aquatic therapy in warm water. | Improves cardiovascular health without overloading joints. Warm water soothes stiffness. Wikipedia+2Southgate Physio+2 |
| Manual Therapy | Joint mobilisation, soft tissue massage to improve movement and reduce pain. | Directly targets stiffness, helps tissues relax. |
| Pain Relief Modalities | Heat packs, cold therapy, TENS units, ultrasound. | Reduces inflammation, calms flare‐ups. |
| Functional Training | Doing movements you actually need: stairs, standing up from chairs, reaching overhead. | Makes daily life easier, retrains body for what you actually do. |
Lifestyle Factors That Influence Arthritis
While you can’t change your age or genetics, there’s a lot you can do to influence how arthritis feels day to day. Carrying extra body weight puts more load on your hips, knees and ankles, speeding up wear and tear. Smoking and poor diet may worsen inflammation, while regular low-impact movement helps lubricate joints and keep muscles strong. Pairing lifestyle tweaks with physio can make your results faster and longer lasting.

How Physiotherapists Assess Arthritis
Your first session isn’t just a quick chat and a stretch. We take a full history of your symptoms, previous injuries, medical conditions and lifestyle. Then we check your posture, walking pattern, joint range of motion and muscle strength. This comprehensive assessment means your physio plan is truly tailored to you — no cookie-cutter routines here.
Home Strategies Between Appointments
What you do between sessions is just as important as what happens in the clinic. Simple habits like using heat or ice packs at the right times, wearing supportive footwear, pacing your activities and doing your prescribed stretches all help you progress. We’ll give you a clear home plan so you know exactly what to do when you’re not with your physio.
When Arthritis Needs More Than Physiotherapy
Physiotherapy is incredibly effective for most people, but sometimes arthritis requires extra help. If you have sudden swelling, severe pain, a new deformity or symptoms that aren’t improving, we’ll liaise with your GP and refer you to a rheumatologist or orthopaedic specialist if needed. This team approach means you get the right care at the right time, without delays.

Real Patient Example from Frenchs Forest NSW Area
I’m seeing lots of people from suburbs around Frenchs Forest, NSW, and one patient stands out:
“Margaret, from Forestville, came in complaining of hip and knee stiffness first thing in the morning, so bad she avoided walks and couldn’t tie her shoelaces without pain.”
After a full physio assessment, we customised her physio plan: daily stretches for hip flexors and hamstrings, strengthening glutes and quads, aquatic therapy sessions twice a week, plus some manual hip mobilisation and advice on posture and joint protection.
Outcomes after 8 weeks:
- Morning stiffness reduced by ~60%.
- Pain dropped from 7/10 to 3/10 most days.
- She could walk 30-minutes around her block without needing to stop.
- Picking up dropped items no longer made her wince.
That’s the power of consistent physio + doing the homework.
Tips to Maximise Your Progress
To get the most out of physiotherapy:
- Be consistent — those exercises you do at home count.
- Start slow and gradually increase intensity. Don’t overdo it.
- Listen to your body — pain is different from discomfort. Sharp, worsening pain is a signal to pull back.
- Keep moving — even small amounts matter (walking, gentle movement).
- Adjust your environment — use supportive footwear, ergonomic setups, aids if needed.
- Stay in touch with your physio — periodic check-ins help adjust things as you improve or if something changes.
When to See a Physiotherapist
You should consider seeking physiotherapy if:
- You’ve noticed persistent joint stiffness lasting more than 30-60 minutes after rest.
- Your joints are painful when moving or weight bearing.
- Stiffness or pain are stopping you doing things you enjoy.
- You notice changes in gait, balance, or do things differently to avoid pain.
- Over the counter meds, rest or heat aren’t helping much.

Benefits vs Other Treatments
Compared to surgery or heavy medication, physio
- Is non-invasive.
- Has fewer side effects.
- Can often reduce the dose or need for certain pain medications.
- Helps with long-term joint health and function, not just temporary relief.
That said, physio often works best in combination with medical care for some types of arthritis—especially inflammatory types or when damage is advanced.
If you have already had a replacement and need help after the operation, CLICK HERE
Summary
If joint stiffness is stopping you from playing with grandkids, doing your job, or enjoying walks, arthritis physiotherapy could be your best natural route. Through tailored exercises, manual therapy, and ongoing support, it’s possible to regain movement, reduce pain, and feel more like yourself again.
Don’t just accept stiffness as “part of ageing.” Make a change.
Give us a call today on 9806 3077, or book online, just CLICK HERE.
References & Further Reading
- Versus Arthritis – Physio Benefits and how it can help Versus Arthritis
- The Chartered Society of Physio – Arthritis condition overview CSP
- PhysioEd – Beyond Pain Relief: The Benefits of Physical Therapy for Arthritis Physio Ed.
- Total Health Clinics Blog – How Physio Can Help Manage Arthritis Total Health Clinics
Give us a call today on 9806 3077, or book online, just CLICK HERE
Living with chronic fatigue can feel like dragging yourself through molasses—constant tiredness, brain fog, sore joints, and rest never seems enough. But gentle physiotherapy can help you regain energy, improve mobility, and ease symptoms without pushing your body into a crash. Read on to discover how tailored movement, pacing, and compassionate care can make all the difference—and see how one local patient from a suburb near Frenchs Forest NSW got better with us. Want to feel more alive again? Let’s get moving (gently).
What is Chronic Fatigue?
Chronic fatigue (often referred to in clinical terms as Myalgic Encephalomyelitis / Chronic Fatigue Syndrome, or ME/CFS) is a complex, long-term condition. It’s not just “feeling tired”—you get overwhelming exhaustion that doesn’t improve with rest, cognitive impairments (“brain fog”), sleep issues, pain, and sometimes worsened symptoms after physical or mental exertion (post-exertional malaise).
Because the causes are multi-factorial (immune, neurological, autonomic dysregulation, inflammation, etc.), recovery tends to be gradual, with ups and downs. The good news? Physiotherapy plays a key role in managing symptoms, improving quality of life, and helping people regain a bit more control.

Who Commonly Gets Chronic Fatigue?
Chronic fatigue can affect anyone, but some groups are more likely to experience it. It’s most often seen in:
- Women between 20–50 years (though men and older adults can also be affected).
- People following viral infections or prolonged illness, where the immune system and nervous system may remain dysregulated.
- Those under high stress or with poor sleep, which can worsen symptoms or act as triggers.
- Individuals with hypermobility spectrum disorders (HSD), hypermobile Ehlers-Danlos syndrome (hEDS) and related conditions. Research shows these groups often experience significant fatigue that is distinct from, but can overlap with, syndromes like ME/CFS. The exact relationship is complex and not fully understood, but issues such as autonomic dysfunction, joint instability and chronic pain are thought to play a role. To learn more about hypermobility CLICK HERE.
Because these factors vary from person to person, it’s important to have a personalised assessment. A physiotherapist familiar with chronic fatigue and hypermobility can help you manage symptoms safely, protect your joints, and pace your activity without worsening your fatigue.

Why Gentle Movement Matters
You might think: if I’m always tired, shouldn’t rest be the priority? Yes, rest is essential. But too much inactivity can lead to deconditioning (muscles weaken, joints stiffen, cardiovascular fitness drops), which actually worsens fatigue and reduces your ability to do the things you want.
Gentle movement helps by:
- Maintaining joint range of motion and preventing stiffness.
- Supporting circulation, which helps with oxygen delivery and removal of metabolic wastes.
- Helping mood, sleep, and relieving anxiety, all of which feed into energy levels.
- Encouraging breathing mechanics and posture, which may help autonomic regulation.
Yet, it’s a fine balance—overdoing it can trigger flare-ups. That’s why pacing, appropriate progression, and individualisation are key.

What Physiotherapy Actually Looks Like
Here are the kinds of things a physiotherapist experienced with chronic fatigue might do:
| Component | What It Involves | Benefits |
|---|---|---|
| Assessment | Listening to your history, understanding your fatigue levels, patterns of exacerbation, what you can tolerate. Possibly use fatigue scales, measure movement or strength baseline. | Helps tailor treatment safely; avoids pushing into “post-exertional malaise.” |
| Pacing & Energy Management | Teaching you how to track energy, schedule rest and activity, avoid boom-bust cycles, find your “energy envelope.” | Prevents crashes; helps you gradually do more without worsening symptoms. |
| Gentle Movement & Stretching | Light stretching, range-of-motion work, possibly bed-based or sitting-based movements; maybe very short walks or gentle mobility exercises. | Keeps joints supple, reduces stiffness, maintains basic mobility. |
| Low Load Strength & Stability | Very light resistance or resistance bands, isometric exercises, focusing on functional tasks rather than high intensity. | Helps preserve muscle strength so daily activities are easier. |
| Breathing, Relaxation & Mind-Body Work | Diaphragmatic breathing, mindfulness, perhaps yoga or Tai Chi modified to fit your energy levels. | Calms nervous system, improves sleep, reduces anxiety. |
| Education & Support | Helping you understand fluctuations, triggers, self-monitoring, setting realistic goals, being kind to yourself. | Empowers you; gives tools to self-regulate and avoid feeling like you’ve failed when symptoms spike. |
What Is Not Helpful
It’s just as important to know what to avoid:
- Rigid graded exercise prescribed without regard for how you’re doing (this can worsen symptoms).
- Pushing through pain or exhaustion; doing more on good days and paying for it with bad crashes.
- Comparing your recovery to others—it’s individual.
- Ignoring signs of overexertion, like worsening fatigue, body pain, cognitive decline, or sleep disturbance.

Clinical Evidence & Best Practices
- Many clinical guides (e.g. 25% ME Group) stress tailored, gentle movement, pacing, and avoiding overexertion. (25% M.E Group)
- Recent blogs and physiotherapy experts highlight that while rest has its role, inactivity leads to decline. Gentle, supervised, gradual movement reduces stiffness, maintains mobility, and supports quality of life. (Active Silvers)
- Movement types like chair yoga, aquatic therapy, breathwork, stretches, mobility especially if done well-paced and respectful of energy levels often show better tolerance. (Active Silvers)
A Local Case Example
Here at our clinic in Frenchs Forest, NSW, we recently saw “Margaret,” who lives in neighbouring Terrey Hills. She had been dealing with chronic fatigue for nearly 18 months. She reported constant fatigue, difficulty walking more than a few minutes, poor sleep, and struggling to keep up with daily chores.
What we did:
- Started with a thorough assessment: fatigue diary, mobility, gentle strength baseline (sit-to-stand, light core work), breathing patterns.
- Introduced pacing: Margaret learned to break tasks into smaller pieces, rest in between, plan good days and bad days.
- Movement plan: seated and lying down stretches; gentle range-of-motion work for shoulders, hips, ankles; breathing and posture work; very gradual walking (starting 2 minutes, twice a day, flat surfaces).
- Added in relaxation and mindfulness to help sleep and calm her nervous system.
Outcome: Over 10 weeks, Margaret’s fatigue severity dropped (she reported fewer “bad crash” days), sleep improved, she could walk 10-12 minutes without needing to stop frequently, she regained confidence to do light household tasks. She still has tough days, but has vastly more energy and function than when she first came to us.
How to Start Gentle Movement Safely
If you suspect you have chronic fatigue, or you already do, here are steps to begin moving gently and safely:
- See a physiotherapist who understands chronic fatigue / ME/CFS.
- Begin with baseline – what can you currently tolerate without feeling worse the next day? Use that as your starting point.
- Track your energy and symptoms (diary, app) so you can see what helps, what hurts.
- Set very small goals (e.g. 2-minute walk, seated stretch) rather than big fitness goals initially.
- Build in rest before, during, and after movement. If you feel worse after an activity, reduce or back off.
- Modify movement: seated rather than standing, lying rather than upright, shorter durations. Use supports (pillows, chairs, walls).
- Incorporate breathwork and relaxation which often help more than we expect.
- Review & adjust often – what works may change week to week, as symptoms fluctuate.

Common Gentle Movement Ideas (You Can Try)
- Seated chair yoga or simple seated stretches
- Bed-based range-of-motion when mobility is low
- Short gentle walks on flat ground
- Water-based movement if access is possible
- Light resistance using bands or isometric holds
- Gentle tai chi or modified yoga with props
- Deep breathing / diaphragmatic breathing, guided relaxation
When to Seek Help / Signs Something’s Wrong
You should contact a health professional (physio, doctor, specialist) if:
- You have symptoms suggestive of chronic fatigue and no diagnosis.
- There is dramatic worsening after any movement/activity.
- There are red-flag signs (e.g. unexplained weight loss, severe pain, neurological symptoms).
- Your fatigue is interfering significantly with life, sleep, mood.
FAQs
Below are some of the FAQs people often ask when thinking about physiotherapy and chronic fatigue.
Frequently Asked Questions
- What kind of physiotherapy is best for chronic fatigue?
The best physio for chronic fatigue is one who offers gentle, individualised care—someone who understands pacing, energy envelope work, uses low-impact movement, and avoids rigid exercise plans that force pushed exertion. - Can gentle exercise make chronic fatigue worse?
Yes, if it’s done without care. Overdoing things, ignoring rest, pushing through fatigue, or using standard exercise programs not adapted to your energy levels can lead to post-exertional malaise (a worsening of symptoms). The trick is gradual, paced, and responsive. - How much and how often should I move if I have chronic fatigue?
Start very small—maybe a few minutes a day, or even multiple short bouts. It depends on how you’re doing. The frequency might increase slowly, always with rest built in, and adjusting depending on how your body responds. There’s no one size fits all. - What is pacing and why is it important?
Pacing means managing your activity and rest to avoid crashes. You balance what feels safe, monitor your energy, plan for rest, and stop before you hit your limit. It helps prevent the boom-and-bust cycles many with chronic fatigue experience. - Are there types of movement or physiotherapy I should avoid?
Yes—high-intensity workouts, strict graded exercise regimes without individualisation, high-load strength training too soon. Anything that causes your symptoms to worsen or doesn’t account for how you feel should be avoided or modified.
Next Steps: How We Can Help You
If you’re reading this and thinking, “Yes, this sounds like me,” you don’t have to stay stuck. Physiotherapy isn’t a magic cure, but it can be a huge part of finding more energy, doing more of what matters, and getting back control over your body rather than letting fatigue control you.
Give us a call today on 9806 3077, or book online, just CLICK HERE to set up a consult. We’d love to walk this journey with you—as gently, thoughtfully, and powerfully as your body allows.
References & Further Reading
- PT for Chronic Fatigue Syndrome – Gentle Exercises for Sustained Energy. Healix Therapy. Healix Therapy
- 5 Best Gentle Exercises For Chronic Fatigue Management. Active Silvers. Active Silvers
- Physiotherapy for ME/CFS: Questions and Answers. 25% ME Group. 25% M.E Group
- How Physical Therapy Can Help Manage Chronic Fatigue Syndrome … Rebuilding Energy, Function and Hope. Witte Physical Therapy. wittephysicaltherapy.com
Sick of constant headaches slowing you down? Have you tried physiotherapy? its more than just a quick fix—it gets to the root cause. From neck tension to posture problems, physios use proven hands-on treatments and tailored exercises to provide long-term relief. Keep reading to learn how we help patients just like you reclaim their day, pain-free.
Why Choose Physiotherapy Over Quick Fixes?
It’s tempting to reach for painkillers when a head pain strikes. But while medication may temporarily dull the pain, it doesn’t solve the underlying problem. They often return because the true cause hasn’t been addressed.
That’s where headache physiotherapy stands out. Instead of masking the pain, physios take a whole-body approach. We investigate your posture, muscle tightness, joint mobility, lifestyle habits, and even stress levels to understand what’s really driving them.
The result? Not only fewer bouts of pain but also improved posture, enhanced movement, less reliance on medication, and a greater sense of control over your own health.

Common Causes of Headaches Treated with Physiotherapy
Physiotherapists are trained to identify musculoskeletal issues that contribute to head pain. Here are the most common culprits we see in clinic:
1. Cervicogenic
These will originate from the neck. Tight muscles, stiff joints, or poor alignment in the cervical spine can send pain signals up to the head. Patients often describe pain starting at the back of the skull and radiating forward.If you’d like to dive deeper into this topic, check out our detailed blog on Neck Pain Physiotherapy.
2. Tension-Type
Stress, fatigue, and long hours at a desk can trigger tightness in the shoulders, neck, and scalp muscles. This leads to a dull, pressure-like pain in the head that feels like a “band” across the head.
3. Postural
“Tech neck” and sedentary lifestyles are a growing issue. Spending hours hunched over a screen strains the neck and upper back, leading to frequent pain that worsen as the day goes on.
4. Jaw (TMJ) Related
Teeth grinding, jaw clenching, or misalignment in the temporomandibular joint can create referred pain into the head. Physiotherapy can address jaw mechanics and reduce tension.
5. Whiplash-Related
Past accidents, even minor ones, can leave a lasting impact. Whiplash injuries often cause long-term neck stiffness and pain in the head if not properly treated.
By addressing these root causes, physiotherapists provide targeted and lasting relief.

How Physiotherapists Treat Headaches
Every patient’s story is unique. That’s why treatment is always tailored. Here’s how we typically approach it:
Manual Therapy
Hands-on techniques such as joint mobilisation, massage, and trigger point release help restore movement and reduce pain. For many patients, manual therapy provides immediate relief.
Dry Needling
Targeting tight trigger points in the neck and shoulder muscles can release tension and decrease referred pain into the head.
Postural Retraining
Poor posture is one of the most common contributors to pain in the head. Physios teach you how to adjust your desk setup, use ergonomic chairs, and maintain better sitting and standing positions.
Exercise Prescription
Targeted stretches and strengthening exercises help support long-term results. For example:
- Stretching the chest muscles to reduce rounded shoulders
- Strengthening the deep neck flexors to improve head positioning
- Shoulder blade stabilisation exercises to support upright posture
Stress Management and Lifestyle Advice
Stress often plays a major role with feeling pain in the head. Physios can provide strategies like breathing techniques, relaxation drills, and advice on sleep posture to reduce triggers.
This multi-faceted approach is what makes physiotherapy so effective.

Example: A Patient’s Journey to Relief
Recently, a patient from Brookvale, just a short drive from our clinic in Frenchs Forest NSW, came in with persistent head pain that had troubled them for over six months. They described a dull ache at the base of the skull that often spread to the temples. Working long hours at a computer made things worse, and painkillers were no longer cutting it.
After a thorough assessment, we discovered their pain was postural in origin, caused by stiffness in the upper neck and weakness in the deep neck stabilisers. Treatment included:
- Manual therapy to loosen stiff neck joints
- Dry needling to release tight trigger points in the shoulders
- A home program of postural exercises and ergonomic adjustments
After just three sessions, their headaches reduced in frequency and intensity. By the sixth session, they were completely pain-free, sleeping better, and no longer relying on daily medication. Today, they maintain their results with a simple at-home program.
The Benefits of Physiotherapy
Patients who commit to physio often experience life-changing improvements, including:
- Reduced frequency and severity of pain – Less disruption to daily life.
- Better posture and body awareness – Especially important for desk-based workers.
- Improved sleep quality – Less tension at night, leading to more restful sleep.
- Increased energy and productivity – No more “lost” afternoons battling pain.
- Less reliance on medication – A safe, drug-free alternative.
- Greater confidence in managing symptoms – Patients feel empowered, not helpless.
For many people, the biggest benefit is freedom—the ability to enjoy work, family, and hobbies without the constant shadow of pain.

Can Physio Prevent Headaches from Returning?
Yes. While quick fixes may temporarily mask symptoms, physio focuses on long-term prevention. By addressing posture, strengthening weak muscles, and providing education on triggers, patients often experience lasting results.
Think of it this way: instead of fighting pain every week, you’re building resilience so they simply don’t come back.
When to See a Physiotherapist for Head Pain
You don’t have to live with recurring head pain. Book in with a physiotherapist if:
- They occur more than once a week
- Painkillers only provide short-term relief
- You notice pain in the head linked to posture, screen use, or stress
- Neck stiffness, jaw pain, or shoulder tension accompany your pain in the head
- Head pain affecting your work, study, or sleep
Early treatment is always best—don’t wait until they become overwhelming.
When You Need Medical Attention (Red Flags)
While many patients respond well to physio, some require urgent medical review. It’s important to know the warning signs:
- Sudden, severe “thunderclap” – Head pain comes on quickly and intensely.
- Head pain with fever, nausea, or stiff neck – Could indicate infection or meningitis.
- New head pain in people over 50 that is not mechanical– Needs investigation for underlying causes.
- Associated head injury – Especially if symptoms worsen or new signs appear.
- Changes in vision, speech, balance, or weakness – Seek medical attention immediately.
- Steadily worsen despite treatment – May need referral for scans or specialist input.
If you experience any of these symptoms, consult your GP or seek urgent care. Physio works best once serious medical conditions are ruled out.

Headache Physiotherapy FAQs
What types of headaches can physiotherapy treat?
Physiotherapy is effective for cervicogenic headaches, tension-type, postural, and those related to jaw dysfunction or whiplash.
How many sessions will I need?
It varies by patient. Some notice results after just 2–3 sessions, while others require a few weeks of consistent care for long-term change.
Is headache physiotherapy safe?
Yes. Physiotherapy is a safe, drug-free, and evidence-based approach tailored to your condition.
Do I need a referral to see a physiotherapist?
No referral is needed—you can book directly with our clinic today.
Can physiotherapy replace medication?
Physiotherapy often reduces reliance on medication, but always consult your GP before adjusting prescribed treatments.
Don’t let pain in your head control your life. Our team at X Physio in Frenchs Forest is here to help you find lasting relief. Give us a call today on 9806 3077, or book online, just CLICK HERE.
References
AI and physiotherapy are reshaping recovery in 2025. From apps to wearables, digital tools are making rehab smarter, faster, and more personalised. In this blog, we’ll explore how technology is improving treatment outcomes, share a local success story, and explain why patients in Frenchs Forest are choosing AI-driven physiotherapy. Ready to accelerate your recovery? Let’s get started.
The Rise of AI and Physiotherapy
Physiotherapy has always been grounded in hands-on care and clinical expertise. But in 2025, AI and physiotherapy are combining to offer more accurate assessments, personalised exercise plans, and better recovery tracking.
Why AI in Physiotherapy Matters
- Personalisation: AI adapts treatment plans to your unique recovery stage.
- Accessibility: Rehab apps put physiotherapy in your pocket.
- Data-driven insight: AI can spot weaknesses and risks even before you feel pain.
- Engagement: Apps and wearables keep patients consistent and motivated.

How AI Is Enhancing Physiotherapy
Artificial Intelligence is playing a powerful role in several areas of physiotherapy care:
- Assessment: Motion sensors and AI-powered cameras can identify subtle movement deficits.
- Treatment Planning: AI systems recommend exercise progressions based on your progress.
- Tracking & Adjustments: Smart platforms notify physiotherapists if your exercises need modification.
This means patients now benefit from faster, more targeted recovery compared to traditional methods alone. When finding a physiotherapist to work with, it is important to consider if the company are keeping up to date with the latest technology on the market to efficiently treat your injury.

Physiotherapy Apps: Your Recovery Companion
Apps are bridging the gap between in-clinic sessions and at-home rehab. At X Physio, we integrate AI and physiotherapy apps to keep patients engaged every day.
Key features include:
- Daily reminders to keep you on track.
- Video demonstrations to improve technique.
- Progress tracking so you can see improvements.
- Telehealth integration for check-ins without leaving home.
Patients often say using a physiotherapy app feels like having their physio with them 24/7.

Wearables and AI: Real-Time Recovery Support
AI and physiotherapy are also merging through wearable technology. Devices can now track:
- Step counts and distances walked
- Posture and movement quality
- Heart rate during exercise
- Sleep quality for recovery support
This data is shared with physiotherapists, allowing for evidence-based decisions and motivating progress. We specifically like to use pedometres when we rehab any lower limb tendon injuries. They come in handy as we can calculate the exact amount of load in a given day which can determine our patient’s walking capacity and keep within the desired load. To learn more about tendon injuries CLICK HERE.

Real-Life Patient Success Story
Recently, we worked with Sarah, a 38-year-old from Oxford Falls near Frenchs Forest NSW, who came to our clinic with knee pain after a netball injury. She’d tried rest, but the pain kept returning.
We combined hands-on physiotherapy treatment with a rehab app powered by AI features that reminded her of exercises, tracked progress, and provided feedback. Sarah also shared wearable data so we could fine-tune her plan. Sarah especially appreciated our use of this App because she was travelling for work for one month and we were able to upgrade the exercises whilst she was away so no time was wasted on her rehab journey.
Eight weeks later, Sarah was back playing netball pain-free, stronger, and more confident. She said the blend of AI and physiotherapy kept her motivated and accountable.
Benefits of AI and Physiotherapy
- Consistency: Apps keep you on track with daily rehab.
- Personalisation: AI ensures exercises match your stage of recovery.
- Faster Results: Data-driven adjustments speed up return to activity.
- Confidence: Patients feel supported between clinic visits.
- Engagement: Recovery becomes interactive and rewarding.
Challenges of AI in Physiotherapy
While AI and physiotherapy are a powerful combination, digital tools are not a substitute for expert care. Manual therapy, clinical judgement, and human connection remain essential. Technology should always complement—not replace—the physiotherapist’s expertise.
The Future of AI and Physiotherapy
We’re only at the beginning. Expect to see:
- Virtual reality rehab for immersive recovery exercises.
- AI-powered injury prevention detecting risks before they happen.
- Greater telehealth integration for patients across rural Australia.
At X Physio, we’re excited to keep blending human expertise with the best of AI and physiotherapy to help our patients in Frenchs Forest and beyond achieve faster, more reliable recoveries.
FAQs: AI and Physiotherapy
Q1: Are AI and physiotherapy tools safe to use for recovery?
Yes—when supervised by a qualified physiotherapist. AI and apps support your rehab journey but don’t replace professional treatment.
Q2: Do I still need to come into the clinic if I use a physiotherapy app?
Definitely. Apps are a supplement, but in-clinic sessions provide manual therapy, assessments, and exercise progressions.
Q3: How does AI personalise my physiotherapy plan?
AI analyses your progress and adapts exercises, while your physio ensures everything remains safe and effective.
Q4: What if I’m not confident with technology?
No worries! We’ll show you how to use the app. Most platforms are designed to be simple and user-friendly.
Q5: Does your Frenchs Forest clinic use AI and physiotherapy apps?
Yes—we use a mix of apps, AI insights, and wearable data to support our patients’ recovery and keep them motivated.
References
- PhysiApp – Guided Exercise Programs
- AI in Physiotherapy Research – Frontiers in Rehabilitation Sciences
- Australian Physiotherapy Association – Digital Health
Give us a call today on 9806 3077, or book online, just CLICK HERE.
{
“@context”: “https://schema.org”,
“@type”: “FAQPage”,
“mainEntity”: [
{
“@type”: “Question”,
“name”: “Are AI and physiotherapy tools safe to use for recovery?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Yes—when supervised by a qualified physiotherapist. AI and apps support your rehab journey but don’t replace professional treatment.”
}
},
{
“@type”: “Question”,
“name”: “Do I still need to come into the clinic if I use a physiotherapy app?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Definitely. Apps are a supplement, but in-clinic sessions provide manual therapy, assessments, and exercise progressions.”
}
},
{
“@type”: “Question”,
“name”: “How does AI personalise my physiotherapy plan?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “AI analyses your progress and adapts exercises, while your physio ensures everything remains safe and effective.”
}
},
{
“@type”: “Question”,
“name”: “What if I’m not confident with technology?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “No worries! We’ll show you how to use the app. Most platforms are designed to be simple and user-friendly.”
}
},
{
“@type”: “Question”,
“name”: “Does your Frenchs Forest clinic use AI and physiotherapy apps?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Yes—we use a mix of apps, AI insights, and wearable data to support our patients’ recovery and keep them motivated.”
}
}
]
}
Sports physiotherapy at XPhysio is specifically available to help athletes and active individuals recover from injuries, prevent setbacks, and perform at their best. Whether you’re chasing goals on the field, the court, or the stage, our expert team provides tailored treatments and support. In this blog, we’ll uncover how our clinic partners with local specialists, sporting clubs, and communities to keep you moving strong.
Why Sports Physiotherapy Matters
Sports can be tough on the body. From muscle strains to ligament tears, the demands of training and competition can leave athletes sidelined. That’s where sports physiotherapy steps in. Our job is to:
- Diagnose and treat sports injuries.
- Develop recovery programs that speed up healing.
- Provide strength and conditioning strategies to reduce re-injury risk.
- Support athletes in returning to peak performance.
It’s more than just injury management — it’s about helping you thrive in sport and life.
If you would like to learn more about our athlete screening, CLICK HERE.

Sports Physiotherapy In Sydney: Our Approach
Our clinic takes a personalised and evidence-based approach to sports physiotherapy. Every athlete is different, which means every treatment plan is too.
Key elements of our approach include:
- Comprehensive Assessment
- Identifying the root cause of your injury, not just treating symptoms.
- Hands-On Treatment
- Manual therapy, dry needling, and joint mobilisation when needed.
- Rehabilitation Programs
- Tailored exercise plans to rebuild strength, flexibility, and endurance.
- Performance Optimisation
- Strategies to improve agility, balance, and overall sporting performance.
- Close Collaboration with Specialists
- We work closely with local sports physicians and orthopaedic specialists who specialise in sporting injuries, ensuring you get the most comprehensive care available.
To learn more about our Sports Physiotherapy – CLICK HERE

Sports Physios Who’ve Lived the Athlete Experience
One thing that sets our team apart is that our physiotherapists have experienced sport first-hand. Many of us have competed at a high level in various sporting codes and know exactly what it’s like to push the body to its limits.
Beyond competing, our physios have also provided treatment and injury support to professional and semi-professional athletes across multiple sports, including rugby, gymnastics, football, athletics, and baseball. This gives us a unique insight into both the physical and mental challenges athletes face during injury and recovery.
When you see us, you’re working with people who’ve been in your shoes — and know what it takes to get back to peak form.

Supporting Sydney’s Local Sporting Community
We’re proud to be deeply connected to the sporting culture of Sydney’s Northern Beaches. Our team works closely with a number of local clubs, including:
- Aussie Gems Dance, Gymnastics and Cheerleading
- Forest Baseball
- Wakehurst Tigers
- Belrose Eagles
- Forest Rugby
Through these partnerships, we provide physiotherapy support for athletes across a wide range of sports — from high-impact football to the artistry of gymnastics and cheerleading.
Our involvement means we don’t just treat injuries — we understand the physical demands of each sport and help athletes build resilience to perform at their best.
Case Example: Success Story from a Local Athlete
Recently, we treated Emily, a 16-year-old gymnast from Killarney Heights, a surrounding suburb of Frenchs Forest NSW. Emily came to us with persistent ankle pain that was limiting her ability to train and compete.
After a thorough assessment, we diagnosed her with ankle impingement caused by repetitive landings. Through a mix of manual therapy, targeted strengthening, and sports-specific rehab exercises, Emily not only overcame her pain but also improved her landing mechanics.
Within eight weeks, she was back training with her club at Aussie Gems — stronger and more confident than ever. This is just one example of how sports physiotherapy Sydney can change the game for athletes.
Sport-Specific Injury Insights
Every sport has its unique physical demands. Here are some of the most common injuries we see in Sydney’s local clubs — and how we tackle them.
🏉 Rugby (Forest Rugby, Belrose Eagles, Wakehurst Tigers)
Rugby is a high-contact sport with a high rate of:
- Shoulder dislocations
- Concussions
- Knee ligament injuries (ACL, MCL)
- Hamstring strains
How we help:
- Strength programs for hamstrings, quads, and shoulders.
- Concussion management and return-to-play protocols.
- Tackling mechanics and injury-prevention education.
🤸 Gymnastics & Cheerleading (Aussie Gems)
Athletes in gymnastics and cheerleading often face:
- Ankle sprains
- Wrist injuries
- Lower back pain from repetitive tumbling
- Overuse injuries in knees
How we help:
- Landing mechanics retraining.
- Wrist and core strengthening.
- Flexibility programs to balance strength and mobility.

⚾ Baseball (Forest Baseball)
Baseball athletes frequently experience:
- Rotator cuff strains
- Shoulder impingement
- Elbow overuse injuries (thrower’s elbow)
How we help:
- Shoulder stability and rotator cuff strengthening.
- Throwing mechanics analysis.
- Gradual return-to-throw programs.

⚽ Football (Wakehurst Tigers)
Football demands explosive speed and constant direction changes, often leading to:
- Groin strains
- ACL and meniscus injuries
- Ankle sprains
How we help:
- Agility and balance retraining.
- Neuromuscular control drills.
- Structured return-to-sport progression after ligament injuries.
Common Sports Injuries We Treat
Some of the most frequent injuries we see in our clinic include:
- ACL injuries (knee ligament tears)
- Hamstring strains
- Shoulder dislocations and rotator cuff injuries
- Tennis elbow and golfer’s elbow
- Shin splints and stress fractures
- Ankle sprains and Achilles tendinopathy
Each injury requires a unique plan, but the goal is always the same — to get you back doing what you love.
Prevention is Just as Important as Recovery
A big part of our role in sports physiotherapy Sydney is preventing injuries before they happen. We do this by:
- Running biomechanical assessments.
- Teaching proper warm-up and cool-down techniques.
- Creating strength and flexibility programs for specific sports.
- Educating athletes and coaches on safe training practices.
When you prevent injuries, you protect your long-term performance and career.
The Extra Edge: Collaboration with Specialists
One of the unique strengths of our clinic is our close relationships with local sports physicians and orthopaedic specialists. If an athlete requires scans, surgical consultation, or specialist input, we streamline the referral process to ensure there are no delays in care.
This integrated approach means you get faster answers, more accurate treatment, and the best possible outcomes.
Why Choose Our Clinic for Sports Physiotherapy Sydney?
- Personalised Care: No cookie-cutter programs — every treatment is customised.
- Community Involvement: We know the local sports scene because we’re part of it.
- Expert Network: Collaboration with sports physicians and orthopaedic specialists.
- Athlete Insight: Our physios have competed at a high level and supported elite athletes.
- Proven Results: Countless athletes from surrounding suburbs like Belrose, Forestville, and Davidson trust us for their recovery.
- Convenient Location: Right here in Frenchs Forest NSW.
FAQs About Sports Physiotherapy Sydney
Q1: What is sports physiotherapy?
Sports physiotherapy focuses on preventing, diagnosing, and treating injuries related to physical activity, sport, and exercise. It also includes performance training and rehabilitation.
Q2: How soon after an injury should I see a sports physio?
Ideally, as soon as possible. Early intervention reduces recovery time and helps prevent chronic issues.
Q3: Do I need a referral to see a sports physiotherapist?
No referral is needed. You can book directly with us. However, we work closely with GPs, sports physicians, and orthopaedic specialists if required.
Q4: Can sports physiotherapy help me if I’m not an athlete?
Absolutely. Sports physio isn’t just for elite athletes — it’s for anyone who’s active or has sustained an injury from physical activity.
Q5: What suburbs do you service?
We’re based in Frenchs Forest NSW and regularly see clients from Oxford Falls, Killarney Heights, Allambie Heights, Forestville, Beacon Hill, Narraweena and surrounding areas.
Final Thoughts
Whether you’re aiming to bounce back from an injury, take your performance to the next level, or simply stay active without pain, sports physiotherapy can make all the difference. With strong community ties, expert partnerships, and proven success stories, our team is ready to support you every step of the way.
👉 Give us a call today on 9806 3077, or book online, just CLICK HERE.
References
- Sports Medicine Australia – Injury Prevention
- Australian Physiotherapy Association – Sports Physiotherapy
- Better Health Channel – Physiotherapy
{
“@context”: “https://schema.org”,
“@type”: “FAQPage”,
“mainEntity”: [
{
“@type”: “Question”,
“name”: “What is sports physiotherapy?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Sports physiotherapy focuses on preventing, diagnosing, and treating injuries related to physical activity, sport, and exercise. It also includes performance training and rehabilitation.”
}
},
{
“@type”: “Question”,
“name”: “How soon after an injury should I see a sports physio?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Ideally, as soon as possible. Early intervention reduces recovery time and helps prevent chronic issues.”
}
},
{
“@type”: “Question”,
“name”: “Do I need a referral to see a sports physiotherapist?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “No referral is needed. You can book directly with us. However, we work closely with GPs, sports physicians, and orthopaedic specialists if required.”
}
},
{
“@type”: “Question”,
“name”: “Can sports physiotherapy help me if I’m not an athlete?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Absolutely. Sports physio isn’t just for elite athletes — it’s for anyone who’s active or has sustained an injury from physical activity.”
}
},
{
“@type”: “Question”,
“name”: “What suburbs do you service?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “We’re based in Frenchs Forest NSW and regularly see clients from Belrose, Forestville, Davidson, and surrounding areas.”
}
}
]
}
Osteoporosis is often called the “silent disease” because bone loss usually happens without symptoms—until a fracture occurs. But the good news? Physiotherapy and evidence-based exercise can strengthen your bones, improve balance, and reduce your fracture risk. In this blog, we’ll share key guidelines, real-life results, and practical strategies you can use today.
What is Osteoporosis?
Osteoporosis is a chronic condition where bones become weak and brittle, making them more prone to fractures—even from simple slips, bumps, or everyday activities. In Australia, more than 900,000 people live with osteoporosis, and another 6.3 million have low bone density (osteopenia). While it’s most common in older women, men are also at risk.
The impact isn’t just physical—it can reduce confidence, independence, and quality of life. That’s why early management with physiotherapy and exercise is critical.

Causes and Risk Factors of Osteoporosis
It develops when bone breakdown happens faster than bone building. This process is influenced by a mix of modifiable and unmodifiable risk factors.
🔹 Primary Osteoporosis (Aging)
- Hormonal Changes:
- Women: A sharp drop in oestrogen during menopause accelerates bone loss.
- Men: A gradual decline in testosterone also weakens bone over time.
- Inadequate Mineral Intake: Insufficient calcium and vitamin D reduces bone mineral density (BMD).
🔹 Secondary Osteoporosis (Other Causes)
- Medical Conditions: Hyperthyroidism, hyperparathyroidism, anorexia, celiac disease, and malabsorption disorders.
- Medications: Long-term corticosteroid use, anti-epileptic drugs, and certain cancer treatments can trigger bone loss.
🔹 Lifestyle Factors
- Physical Inactivity: A sedentary lifestyle accelerates bone decline.
- Smoking: Nicotine slows bone-building cells and reduces calcium absorption.
- Excessive Alcohol Intake: More than two drinks per day increases fracture risk.
🔹 Unmodifiable Risk Factors
- Age and Gender: Risk rises with age; women are more susceptible.
- Genetics: Family history of the condition or hip fractures increases likelihood.
- Body Size: Smaller frames start with less bone mass.
- Ethnicity: Higher risk in White and Asian populations.

Evidence-Based Exercise Guidelines for Osteoporosis
Physiotherapy-led exercise is one of the most effective ways to manage osteoporosis and osteopenia. According to recent guidelines, the key recommendations are:
1. Resistance Training
- Frequency: 2–3 times per week
- Structure: 1 set of 5–12 reps across 3–10 exercises
- Equipment: Free weights and machines
- Intensity: 50–85% of 1RM
- Duration: 3–12 months minimum
👉 Targets major muscle groups, improves bone loading, and increases muscle strength to reduce fall risk.
2. Impact Exercise
- Examples: Jump drops, jumping chin-ups with drop landings, jump rope
- Volume: 50 jumps per session
- Frequency: 3+ days per week
- Duration: At least 6 months
👉 Provides direct stimulation to bones, especially useful for hip and spine density.
3. Weight-Bearing Aerobic Exercise
Walking, stair climbing, and light jogging help maintain bone density.
4. Balance Training
Reduces fall risk, improving confidence and safety.
5. Habitual Physical Activity
Staying active in daily life prevents further bone loss.
Important: Every exercise program must be tailored to the individual’s health status, fracture risk, and physical capacity—a key role of your physiotherapist.

How Physiotherapy Helps
At our Frenchs Forest clinic, physiotherapy for osteoporosis includes:
- Designing safe, personalised exercise programs (resistance + impact + balance).
- Teaching correct techniques for lifting, bending, and posture to protect bones.
- Monitoring progress and safety, adjusting exercises as strength improves.
- Providing pain management strategies if fractures or discomfort are present.
- CLICK HERE to learn more about dealing with a chronic condition.

Patient Success Story
We recently treated Maria, a 68-year-old from Forestville, near Frenchs Forest, who was diagnosed with osteoporosis after a wrist fracture from a minor fall.
Maria felt nervous walking outdoors and had poor confidence in her balance. We created a 12-week program combining resistance training, balance drills, and posture work.
- Her leg and core strength improved by 25%.
- She now walks confidently without fear of falling.
- She has joined our ongoing group classes to continue building strength.
Physiotherapy gave Maria not just stronger bones—but independence and confidence to enjoy life again.
Lifestyle Strategies for Osteoporosis
Alongside physiotherapy, you can support bone health with:
- Adequate calcium & vitamin D (from diet or supplements).
- Quitting smoking & reducing alcohol.
- Daily activity—gardening, dancing, or walking.
- Bone scans (DEXA scans) every 2–3 years if you’re at risk.

Myths Busted
- ❌ “Exercise is unsafe if you have osteoporosis.”
✅ In fact, exercise is one of the most important treatments when supervised. - ❌ “Osteoporosis only affects women.”
✅ Men are also at risk, especially over 70. - ❌ “If I don’t have pain, my bones must be fine.”
✅ Osteoporosis is painless until a fracture happens.
FAQs About Osteoporosis and Physiotherapy
Q1: Can physiotherapy reverse osteoporosis?
No. It can’t reverse it, but it slows progression, reduces fracture risk, and improves strength and balance.
Q2: How often should I exercise if I have osteoporosis?
Guidelines recommend 2–3 resistance sessions per week, impact training 3+ days/week, and daily activity.
Q3: Is it safe to lift weights with osteoporosis?
Yes, under physiotherapist supervision. Correctly prescribed weight training strengthens bones safely.
Q4: Do I need a GP referral to see a physio?
No referral needed. You can book directly, though your GP may recommend a DEXA scan or medication too.
Q5: Can physiotherapy help if I’ve already had a fracture?
Yes. Physios provide rehab, pain management, and fall-prevention strategies to stop further injury.
Final Thoughts
Osteoporosis doesn’t have to mean giving up the activities you love. With physiotherapy, tailored exercise, and lifestyle changes, you can strengthen your bones, reduce your fracture risk, and regain confidence in your movement.
👉 Give us a call today on 9806 3077, or book online, just CLICK HERE
References
- Osteoporosis Australia
- Better Health Channel
- Physiopedia
- Zhao R, et al. Exercise Guidelines for Osteoporosis and Osteopenia.
Knee pain can be a real game-changer – it can stop you from running, squatting, climbing stairs, or even enjoying a simple walk around the block. But here’s the good news: with the right physiotherapy treatment in Frenchs Forest, most knee pain can be managed effectively. In this blog, we’ll cover causes, treatment options, and real results we’ve seen in our clinic.
Why Is Knee Pain So Common?
Knee pain is one of the most frequent reasons people book a physiotherapy appointment. Whether you’re an athlete, a tradie, or simply dealing with everyday wear and tear, your knees take on a lot of load.
Common causes include:
- Overuse injuries – running, cycling, or repetitive kneeling.
- Acute injuries – ACL tears, meniscus injuries, ligament sprains.
- Osteoarthritis – age-related wear and tear of cartilage.
- Patellofemoral pain syndrome (runner’s knee) – pain around the kneecap, often worse with stairs.
- Muscle imbalances – weak glutes or quads leading to poor tracking.
- Post-surgical pain – following arthroscopy, ACL reconstruction, or knee replacement.

Real Patient Success Story – Knee Pain Treatment Near Frenchs Forest
Recently, we treated Sarah, a 42-year-old from Forestville, just minutes from Frenchs Forest. She had ongoing knee pain that was stopping her from playing netball and even walking her dog.
After a detailed physiotherapy assessment, we found her pain was linked to patellofemoral joint irritation caused by weak hip muscles and thigh imbalance.
Her personalised treatment plan included:
- Manual therapy and massage to release tight tissues.
- Targeted strengthening for glutes and quadriceps.
- Knee taping techniques for better tracking.
- Education on training loads and recovery.
✅ Within six weeks, Sarah was back on the netball court – pain-free and stronger than before.
How Physiotherapy Helps with Knee Pain
If you’re searching for “knee pain physio near me” in Frenchs Forest, here’s what to expect from treatment:
Step 1: Comprehensive Assessment
Your physio will check movement, strength, flexibility, and joint mechanics.
Step 2: Hands-On Treatment
This may include joint mobilisation, massage, or dry needling to reduce stiffness and pain.
Step 3: Tailored Exercise Program
Custom rehab exercises address weaknesses and improve long-term joint function. Focus areas often include:
- Glute strengthening
- Quadriceps activation
- Core and balance retraining
Step 4: Load Management
We’ll help you stay active while protecting your knee.
Step 5: Prevention & Education
Learn the best footwear, posture, and activity modifications to stop pain returning.

Types of Knee Pain We Treat at X Physio Frenchs Forest
Osteoarthritis of the Knee
- Morning stiffness, grinding, difficulty walking.
- Treatment: Strength training, hydrotherapy, mobility exercises, weight management.
Patellofemoral Pain Syndrome (Runner’s Knee)
- Pain around the kneecap, worse with stairs or squats.
- Treatment: Taping, hip and quad strengthening, movement retraining.
Meniscus Injuries
- Catching, locking, twisting pain.
- Treatment: Stability rehab, gentle loading, post-surgical recovery programs.
- To learn more about meniscus injuries, CLICK HERE
ACL Injuries (Surgical & Non-Surgical)
- Instability, swelling, giving way.
- Treatment: Progressive strength, proprioception training, return-to-sport guidance.
Iliotibial Band Syndrome (ITB Pain)
- Pain on the outer side of the knee.
- Treatment: Tissue release, glute strengthening, running technique correction.

Lifestyle Habits That Worsen Knee Pain
- Sitting too much (weakens supporting muscles).
- Weight gain (adds pressure to joints).
- Poor footwear or worn-out runners.
- Overtraining without recovery.

Self-Management Tips Before Seeing a Physio
- Use ice after flare-ups.
- Wear supportive shoes.
- Strengthen hips and thighs regularly.
- Avoid full rest – keep moving within limits.
- See a physiotherapist early for long-term results.

FAQs – Knee Pain & Physiotherapy
How do I know if my knee pain is serious?
If your knee pain is sudden, severe, or comes with swelling, locking, or giving way, it’s best to see a physiotherapist or GP. Pain lasting longer than a few weeks also needs professional assessment.
Can physiotherapy really help knee arthritis?
Yes. Physiotherapy helps strengthen the muscles around the knee, improve flexibility, and reduce stiffness. Many patients with arthritis report significant pain relief and better mobility with consistent physiotherapy.
Should I rest or exercise with knee pain?
Complete rest often makes knee pain worse. The key is finding the right type and amount of movement. Physiotherapists can guide you with safe, tailored exercises that reduce pain and build strength.
Final Thoughts
Knee pain doesn’t have to control your life. Whether it’s arthritis, sports injuries, or day-to-day aches, physiotherapy offers proven solutions to get you moving again. Just like Sarah from Belrose, you too can bounce back stronger with the right treatment.
👉 Give us a call today on 9806 3077, or book online, just CLICK HERE
References
Neck pain can stop you in your tracks—making it hard to sleep, work, or even enjoy your day. Whether it’s from posture, stress, or an injury, the good news is physiotherapy can help you move freely again. In this blog, we’ll unpack common causes, “tech neck,” sedentary lifestyles, practical strategies, proven physio treatments, and simple exercises you can start today.
Why Neck Pain Is So Common
Neck pain is one of the most frequent issues we treat in clinic. Studies suggest that up to 70% of adults experience neck pain at some stage of their lives. The neck is a complex structure—seven vertebrae supported by muscles, ligaments, and discs. It also carries the weight of your head (around 5kg on average!).
Add modern-day stressors like prolonged desk work, smartphones, and poor posture, and it’s no wonder so many Australians deal with stiffness, headaches, and sharp twinges in their neck.

Common Causes of Neck Pain
- Poor Posture
- Hunching at your desk or looking down at your phone (“tech neck”) places extra strain on neck muscles.
- Muscle Strain
- Overuse from repetitive movements or sudden awkward positions.
- Stress and Tension
- Stress often shows up as tight shoulders and neck stiffness.
- Injury
- Whiplash from car accidents or sports injuries.
- Degenerative Conditions
- Osteoarthritis and disc degeneration can cause pain, stiffness, and reduced mobility.
- To find out more about the disc, please read our blog: Intervertebral Disc: how physiotherapy can help

“Tech Neck” – The Modern Epidemic
“Tech neck” refers to the pain and stiffness caused by constantly looking down at devices like phones, tablets, or laptops.
When you tilt your head forward, the pressure on your neck increases dramatically:
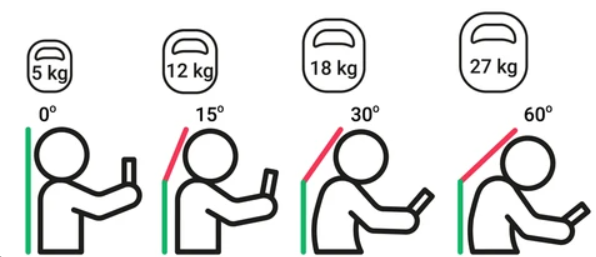
- At a neutral angle, your head weighs around 5kg.
- At a 15-degree tilt, it’s closer to 12kg
- At a 30-degree tilt, it’s closer to 18kg.
- At 60 degrees, your neck is carrying the equivalent of 27kg!
Over time, this leads to muscle fatigue, stiffness, headaches, and even long-term postural changes. Physiotherapy can help retrain your posture, relieve tight muscles, and give you strategies to reduce daily strain.
Sedentary Lifestyles and Neck Pain
Many Australians spend more than 8 hours a day sitting—often at a desk or behind a screen. Prolonged sitting leads to:
- Weak postural muscles (especially deep neck stabilisers)
- Tight chest and shoulder muscles
- Reduced blood flow to spinal tissues
This combination creates the “perfect storm” for neck pain. Movement is medicine, and physiotherapy not only treats the pain but also equips you with active strategies to break the sitting cycle.

Symptoms You Might Notice
- Stiffness when turning your head
- Dull ache or sharp pain
- Pain radiating into shoulders or arms
- Headaches (especially tension headaches)
- Tingling or numbness in arms or hands
- Difficulty sleeping due to discomfort
How Physiotherapy Helps Neck Pain
Physiotherapy treatment is not just about easing the pain—it’s about finding the root cause and preventing flare-ups in the future.
1. Hands-On Treatment
- Gentle joint mobilisation to improve movement.
- Soft tissue massage to ease muscle tightness.
2. Targeted Exercise Programs
- Strengthening weak muscles.
- Stretching tight areas.
- Restoring posture and balance.
3. Postural Education
- Guidance on how to set up your workstation.
- Teaching you simple corrections you can do daily.
4. Pain Relief Modalities
- Heat, cold and sometimes dry needling to release tension.
5. Long-Term Management
- Preventing recurrence with a personalised plan.

Patient Story: How “Sarah” Beat Neck Pain
Sarah, a 42-year-old accountant, came into our clinic complaining of constant stiffness in her neck and headaches that worsened by the end of the workday. She described feeling “locked up” and often reached for painkillers just to get through the week.
During her assessment, we discovered:
- Poor desk ergonomics
- Tight upper trapezius muscles
- Weak deep neck flexors
Her treatment plan included:
- Weekly manual therapy to release tight muscles
- Posture correction and ergonomic advice for her workstation
- A simple daily home exercise program focused on strengthening her deep neck stabilisers
After four weeks, Sarah reported less pain, improved mobility, and most importantly—her headaches had eased significantly. By her eighth week of treatment, she was working comfortably without needing medication.
Sarah’s case shows that with the right approach, physiotherapy can make a huge difference in quality of life.
Best Desk Stretches & Mobility Exercises for Neck Pain
Here are five simple exercises you can do at home or at work to relieve tension and prevent “tech neck.”

- Chin Tucks
- Sit upright, gently tuck your chin back as if making a double chin.
- Hold for 5 seconds, repeat 10 times.
- Strengthens deep neck stabilisers.
- Upper Trapezius Stretch
- Sit tall, tilt your ear towards your shoulder.
- Hold for 20–30 seconds, repeat both sides.
- Stretches the muscles at the side of the neck.
- Levator Scapulae Stretch
- Sit upright, turn your head 45 degrees to the right, then look down towards your armpit.
- Hold 20 seconds, repeat on both sides.
- Great for relieving stiffness.
- Shoulder Blade Squeezes
- Sit upright, pull your shoulder blades back and down.
- Hold for 5 seconds, repeat 10 times.
- Improves posture and reduces forward rounding.
- Neck Rotations
- Slowly turn your head left to right.
- Repeat 10 times each side.
- Keeps your neck mobile throughout the day.
💡 Pro tip: Try setting a timer to remind yourself to move every hour—these mini breaks are just as important as the stretches themselves.
When to See a Physiotherapist
While mild stiffness often resolves with self-care, it’s time to book an appointment if you experience:
- Pain that persists beyond a few days
- Recurring headaches linked to neck tension
- Tingling or numbness in your arms
- Severe or sudden pain after an injury
The Benefits of Physiotherapy for Neck Pain
- Drug-Free Pain Relief
- Restored Mobility and Function
- Reduced Headaches
- Better Posture and Body Awareness
- Long-Term Prevention of Recurrence
Final Thoughts
Neck pain is common—but it doesn’t have to control your life. With physiotherapy, you can address the root cause, relieve discomfort, and prevent future flare-ups. If you’ve been struggling with stiffness, headaches, “tech neck,” or the effects of long hours sitting, now’s the time to take action.
👉 Give us a call today on 9806 3077, or book online, just CLICK HERE.
References
- Better Health Channel – Neck pain
- Physiopedia – Neck pain
- Spine Health – Neck Pain Causes and Treatment
Recovering from shoulder surgery can feel overwhelming, but with the right physiotherapy approach, you can get back to strength, movement, and everyday life sooner than you think. In this blog, we’ll cover what shoulder surgery recovery involves, why physiotherapy is vital, and share a real success story from our clinic. Ready to take the first step to a stronger shoulder? Let’s dive in.
Why Shoulder Surgery Happens
Shoulder surgery is often needed when injuries or long-term issues don’t improve with conservative treatments like rest, medication, or physiotherapy alone. Common reasons include:
- Rotator cuff tears – when the tendons around the shoulder are damaged or torn.
- Shoulder impingement – caused by structures in the shoulder rubbing painfully.
- Labral tears – damage to the cartilage ring that helps stabilise the joint.
- Shoulder instability/dislocation – when the joint keeps slipping out of place.
- Severe arthritis – sometimes leading to shoulder replacement surgery.
Each of these conditions can seriously affect how you move, work, and enjoy life. That’s where surgery—and crucially, physiotherapy afterwards—comes in.
To find out more about Rotator cuff injuries, CLICK HERE

The Role of Physiotherapy After Shoulder Surgery
Surgery might repair the structure of your shoulder, but it’s physiotherapy that helps you regain function. Here’s why it’s so important:
- Reducing pain and swelling – targeted exercises and hands-on treatment can calm things down.
- Restoring movement – gentle, guided exercises to gradually return range of motion.
- Building strength – reactivating weakened muscles to stabilise the joint.
- Improving posture – fixing compensations you may have developed before or after surgery.
- Preventing re-injury – making sure your shoulder recovers stronger than before.
Skipping or delaying physio can slow your recovery and increase the risk of stiffness or weakness becoming long-term problems.

What to Expect: A Timeline for Recovery
Every surgery is different, but here’s a general idea of how recovery phases may look with physiotherapy:
Phase 1: Protection & Pain Relief (0–6 weeks)
- Wearing a sling to protect the repair.
- Gentle passive exercises guided by your physio.
- Focus on pain management, swelling reduction, and posture.
Phase 2: Regaining Movement (6–12 weeks)
- Gradual introduction of active-assisted and active exercises.
- Restoring shoulder mobility and starting light functional tasks.
- Ongoing hands-on treatment to improve soft tissue flexibility.
Phase 3: Strengthening & Control (3–6 months)
- Progressive strengthening of the rotator cuff and surrounding muscles.
- Exercises targeting stability and coordination.
- Returning to more demanding daily tasks and work duties.
Phase 4: Return to Sport or Full Activity (6+ months)
- Higher-level strengthening, power, and agility drills.
- Sport-specific or occupation-specific rehab.
- Preventative strategies to reduce re-injury risk.
Your timeline may vary depending on the type of surgery, your goals, and how your body responds.

Common Challenges During Recovery
Shoulder surgery rehab isn’t always smooth sailing. Some challenges you may face include:
- Stiffness – often from wearing a sling for weeks.
- Weakness – muscles waste quickly after surgery.
- Fear of movement – many people feel nervous about “damaging” their repair.
- Sleep problems – discomfort can interrupt rest.
- Frustration – recovery takes time, and patience is key.
The good news? With consistent physio, most of these challenges can be managed and overcome.

Real Patient Success Story
Recently, we worked with Michael, a 48-year-old tradie from Allambie Heights who underwent rotator cuff surgery after years of shoulder pain from heavy lifting and overhead work.
When Michael first came to us, he was:
- Struggling to move his arm above shoulder height.
- Experiencing pain just trying to dress himself.
- Worried about getting back to work.
We guided him through a structured post-op program:
- Weeks 1–6: Focused on passive range exercises, posture correction, and gentle manual therapy to ease stiffness.
- Weeks 6–12: Introduced active range of motion and light strengthening.
- Weeks 12+: Progressed to targeted strengthening, lifting drills, and functional activities related to his job.
Fast forward six months—Michael is now back on site, lifting tools confidently, and even hitting the gym again. His biggest win? “I can finally sleep through the night without that dull ache in my shoulder,” he told us.
Tips for a Smooth Recovery
Here are some simple yet powerful strategies we recommend to all our patients recovering from shoulder surgery:
- Stick to your physio plan – consistency is everything.
- Don’t rush it – pushing too hard can do more harm than good.
- Prioritise posture – especially if you’re sitting at a desk.
- Stay active in safe ways – gentle walking and lower body exercises can boost recovery.
- Ask questions – your physio is there to guide and reassure you.
Why Choose Physiotherapy With Us?
At our clinic, we pride ourselves on:
- Personalised programs – no cookie-cutter rehab here.
- Hands-on treatment – to ease pain and speed up progress.
- Sports and work-focused rehab – tailored to your goals.
- Ongoing support – guiding you every step of the way.
- Strong Relationships – with local Surgeons
Our team understands the frustration of being sidelined by surgery—and we know how to get you back moving, stronger than ever.

Final Thoughts
Shoulder surgery is just the first step—physiotherapy is what helps you truly get your life back. Whether it’s returning to work, sport, or simply enjoying everyday activities without pain, the right rehab program makes all the difference.
If you’re recovering from shoulder surgery or preparing for one, don’t wait to get started with physiotherapy.
👉 Give us a call today on 9806 3077, or book online, just CLICK HERE.
References
- Better Health Channel – Shoulder Surgery
- Physiopedia – Rotator Cuff Repair https://www.physio-pedia.com/Rotator_Cuff_Repair_RehabilitationRehabilitation
- Healthdirect – Shoulder Problems
- Australian Physiotherapy Association – Why See a Physio?
