Got a pinched nerve in your back and sick of the sharp, burning, or shooting pain running your day? You’re not alone—and the good news is most cases improve with targeted physiotherapy. This blog breaks down what actually works, what doesn’t, and how real patients get back to normal faster. If you’re struggling now, reach out today.
Pinched Nerve in the Back: Physio Treatment Options That Actually Work
A pinched nerve in the back can be one of the most frustrating and painful issues to deal with. Whether it causes sharp lower-back pain, leg pain, buttock pain, numbness, tingling, or weakness, it can stop you from working, lifting, walking, or even sleeping properly. The good news? Most pinched nerves respond extremely well to the right physiotherapy plan—often avoiding the need for injections or surgery.
In this article, we’ll walk you through:
- what a pinched nerve actually is
- the most effective physio treatments (based on current evidence)
- what you shouldn’t do
- a real-life example of a patient from a nearby suburb
- and when you should seek help urgently
If you’re currently dealing with pain, book in and let us help you get moving again.

What Exactly Is a Pinched Nerve in the Back?
A pinched nerve occurs when a spinal nerve becomes irritated or compressed by surrounding structures such as:
- irritated or inflamed discs
- joint swelling
- muscle spasm
- narrowing of spinal canals (stenosis)
- bone or joint changes
- inflammation after lifting or twisting
A Pinched Nerve in the Back becomes sensitive, leading to symptoms such as:
- sharp back pain
- shooting pain into the leg or buttock
- numbness or pins and needles
- muscle weakness
- increased pain with sitting, bending, or coughing
Contrary to the name, the nerve is rarely “trapped permanently”—most cases are due to temporary irritation or inflammation, and the right physio treatment can settle the nerve quickly.

Why Physiotherapy Works So Well for A Pinched Nerve in the Back
Physiotherapy has been shown to be highly effective for A Pinched Nerve in the Back because it targets the mechanical stresses and inflammatory processes behind the irritation.
A well-designed physio plan aims to:
✔ Reduce nerve inflammation
✔ Improve mobility in stiff joints
✔ Reduce pressure on the affected nerve
✔ Strengthen the back, hips, and core
✔ Improve posture and lifting habits
✔ Prevent recurrence
Now let’s break down the treatment options that actually work.
Physio Treatment Options That Actually Work
1. Directional Preference Exercises (Often Used for Disc-Related Pain)
A Pinched Nerve in the Back can come from an irritated disc. Repeated movements in specific directions (often extension-based exercises) can:
- centralise symptoms
- reduce leg pain
- reduce disc pressure
- improve mobility
McKenzie-style exercises are commonly used and are backed by strong evidence for disc pain.
But the key is finding the right direction for your back—doing the wrong one can worsen symptoms, which is why guidance is important.

2. Manual Therapy to Reduce Joint and Muscle Tension
Hands-on therapy helps reduce mechanical loading on A Pinched Nerve in the Back, including:
- joint mobilisation
- soft tissue release
- neural mobility techniques
- trigger point therapy
- gentle manipulation (if appropriate)
These techniques help free up stiff spinal segments and reduce inflammation around the irritated nerve root.
3. Neural Gliding (Nerve Mobility Exercises)
When a nerve becomes irritated, the mobility of the nerve can reduce. Guided nerve glides help the nerve slide and move more comfortably along its pathway. This reduces pain, tingling, and stiffness—especially in the leg.
These must be done gently, or symptoms can flare.
4. Targeted Strengthening for Long-Term Relief
Strengthening is essential to stop symptoms from recurring. For A Pinched Nerve in the Back, we focus on:
- deep core stability
- hip strength
- postural endurance
- glute activation
- spinal stabilisation
As strength improves, the irritated nerve is exposed to less pressure and irritation.
5. Activity Modification — Not Complete Rest
Gone are the days of bed rest. We now know it slows recovery.
Physios guide you in:
- what movements to avoid short-term
- how to keep moving safely
- how to reduce inflammation without stopping your life
- how to gradually reintroduce bending, lifting, or running
This approach almost always leads to faster improvement.
6. Heat, Ice, or TENS for Short-Term Relief
These do not fix the cause but are useful tools to reduce pain temporarily. Your physio will recommend the right one based on your symptoms.
7. Posture and Ergonomic Advice
Pain caused by sitting (especially prolonged slumped posture) is common with disc-related pinched nerves. Small ergonomic adjustments can dramatically reduce symptoms.
8. Load Management for Workers, Runners, or Lifters
If you’re a tradie, gym-goer, or runner, load plays a major role in recovery. A physio will guide how much you can do, and how fast you can increase activity safely.
A Real Patient Example from a Nearby Suburb
Last month, we saw Sarah (name changed for privacy), a 42-year-old office worker from Forestville, just a short drive from Frenchs Forest NSW. She came in with severe lower-back pain and shooting leg pain after lifting a heavy box at home.
Her symptoms included:
- pain down the right leg
- numbness in the calf
- difficulty sitting at work
- sharp pain when bending
After a thorough assessment, we identified a pinched lumbar nerve likely related to a disc irritation. Her treatment plan included:
- directional preference extension exercises
- manual therapy for lumbar stiffness
- nerve gliding for the irritated sciatic nerve
- ergonomic and workstation advice
- progressive strengthening
Within 3 weeks, her shooting pain had resolved. She returned to full-time work comfortably, had better sitting posture, and resumed light gym training. Her long-term program now focuses on deep core and hip strength to prevent recurrence.
Stories like Sarah’s are common—pinched nerves often respond extremely well when treated early and guided properly.
How Long Does It Take to Recover?
Most people see improvements within 1–3 weeks.
Full recovery often takes 4–8 weeks depending on:
- severity
- your job and activity level
- how long symptoms have been present
- adherence to your exercise plan
Chronic or severe nerve compression may take longer, but even long-term cases usually improve significantly with a structured physio program.
When Should You Seek Help Urgently?
Seek immediate medical attention if you experience:
- loss of bowel or bladder control
- numbness around the groin (saddle region)
- severe or rapidly worsening weakness
- unrelenting night pain
These symptoms are rare but require urgent assessment.
When Should You See a Physio?
You should book an appointment if:
- pain is more than mild
- symptoms spread into the leg
- you feel numbness or tingling
- pain has lasted more than 3–5 days
- work, sleep, or walking are affected
- pain keeps coming back
The earlier we treat a pinched nerve, the faster and smoother recovery usually is.
FAQs About Pinched Nerve in the Back
1. How do I know if I have a pinched nerve in my back?
Typical signs include sharp back pain, leg pain, numbness, tingling, or weakness. A physio can assess and confirm the cause.
2. Can a pinched nerve heal on its own?
Yes, many cases improve naturally, but physio speeds recovery, prevents flare-ups, and reduces the chance of chronic nerve irritation.
3. Should I rest or keep moving?
Gentle movement is best. Avoid complete rest. Your physio will guide safe movements that reduce nerve stress.
4. Do I need an MRI?
Not usually. Most cases don’t require scans unless symptoms are severe or not improving with treatment.
5. Can physiotherapy prevent the pinched nerve from returning?
Yes — strengthening, mobility work, and posture education significantly reduce the risk of future episodes.
References
- Australian Physiotherapy Association – Back Pain Resources
https://australian.physio/ - Better Health Channel – Back Pain
https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/back-pain - X Physio Blog – Exercises, Injury Guides & Physio Advice
https://xphysio.com.au/blog/
Give us a call today on 9806 3077, or book online, just CLICK HERE.
{
“@context”: “https://schema.org”,
“@type”: “FAQPage”,
“mainEntity”: [
{
“@type”: “Question”,
“name”: “How do I know if I have a pinched nerve in my back?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Common signs include sharp back pain, shooting leg pain, numbness, tingling, or weakness. A physiotherapist can assess and confirm the cause.”
}
},
{
“@type”: “Question”,
“name”: “Can a pinched nerve heal on its own?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Yes. Many cases improve on their own, but physiotherapy speeds up recovery, prevents ongoing flare-ups, and reduces nerve irritation.”
}
},
{
“@type”: “Question”,
“name”: “Should I rest or keep moving?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Gentle movement is better than complete rest. Your physiotherapist will guide which movements are safe and reduce nerve stress.”
}
},
{
“@type”: “Question”,
“name”: “Do I need an MRI?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Most people do not need an MRI unless symptoms are severe, persistent, or not improving with treatment.”
}
},
{
“@type”: “Question”,
“name”: “Can physiotherapy prevent the pinched nerve from returning?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Yes. Strengthening, postural training, and mobility work help reduce the risk of recurring episodes.”
}
}
]
}
Looking to stay fit and healthy? The simple answer is: aim for about 2½ to 5 hours of moderate exercise — or 1¼ to 2½ hours of vigorous exercise — per week, plus some strength work. Stick around and I’ll show you how to make this work for your lifestyle (even if you’re flat out during the week).
Why Weekly Exercise Matters — And What “Enough” Actually Means
When it comes to staying healthy, moving regularly is key. According to the official guidelines from the Australian Government, adults aged 18–64 should aim to be active most days of the week, building up to either:
- 2.5 to 5 hours per week of moderate-intensity activity (like brisk walking, casual cycling, swimming, or gardening), or
- 1.25 to 2.5 hours per week of vigorous-intensity activity (like jogging, fast cycling, aerobics, or sport), or
- A mix of both.
On top of that, you should include muscle-strengthening activities on at least 2 days per week — things like squats, lunges, push-ups, lifting weights or even heavy housework count.
And if you’re mostly sitting during the day — maybe at a desk job — it’s not enough to just “count the gym.” Minimising prolonged sitting and breaking up long periods of inactivity also matters.
Although this is the general guidelines for most people, certain ages and conditions will require more specific exercise instructions. Read more about our Osteoporosis blog to find out more about this condition’s requirements: HERE

What That Looks Like in Real Life
Okay, so 2.5 to 5 hours a week — what does that really look like when you’re juggling work, kids, errands and maybe a bit of Netflix? Here are some realistic “lifestyle-friendly” examples:
| Goal | Example Plan |
|---|---|
| 150 minutes/week moderate (minimum) | 30 min brisk walk × 5 days (e.g. before/after work, walking to shops) |
| 300 minutes/week moderate (upper guideline) | 30 min brisk walk × 5 days + 45–60 min cycling or swimming on weekend |
| 75 min/week vigorous (minimum vigorous) | 25 min jog × 3 days per week |
| Mixed approach | 2 brisk walks (30 min), 2 gym sessions (45 min), 1 weekend swim or hike |
And for muscle strength — maybe throw in a couple of short bodyweight sessions (squats, lunges, push-ups) on two or more days per week.
If you’re currently doing nothing, that’s totally fine — start small. Even a 10-minute walk each day is better than nothing. The key is consistency, not perfection.
Why These Guidelines Matter (Beyond Just “Looking Fit”)
Meeting these targets doesn’t just help you lose weight or tone up. Regular, appropriately dosed exercise:
- supports heart and lung health, reducing risk of heart disease, stroke and high blood pressure Heart Foundation+1
- helps maintain muscle and bone strength, especially important as we get older Health, Disability and Ageing+1
- lifts mood and mental well-being, improves sleep and reduces risk of chronic disease Health, Disability and Ageing+1
- combats the negative effects of too much sitting — which, even if you “exercise,” can still increase risk of metabolic issues if you sit for long periods.
So really — doing the recommended amount isn’t just about looking good. It’s about feeling good, staying strong, and protecting long-term health.

How to Make It Work — In a Busy Life
If you lead a busy life (work, kids, commitments) — and you live in or around suburbs like ours (we’re based near Frenchs Forest, so many of our patients commute from nearby suburbs) — here are some tips to build movement into your week without overwhelming yourself:
- Treat exercise like brushing your teeth: a little bit every day rather than a big “weekend warrior” session.
- Use active transport where possible — walk or cycle to the shops, hop off the bus a stop early, walk the dog.
- Break up long periods of sitting at work — set a timer every hour to stand up, stretch or walk for 2–5 minutes.
- Combine movement with chores — garden, vacuum, mow the lawn — it counts.
- Find something you enjoy — walking, dancing, swimming, social sport — you’re far more likely to stick with it long-term that way.
- Do muscle-strengthening or mobility exercises twice a week — even short sessions of bodyweight exercises count.
Real Results: A Case from Our Clinic
To make this concrete, here’s a recent example from our physiotherapy clinic:
A patient in their mid-40s came in from a nearby suburb (just a 15-minute drive down from Frenchs Forest). They were complaining of recurring lower-back stiffness and general fatigue — they worked in an office, sat all day, got home late, and had little energy for exercise.
We began by prescribing simple, achievable changes: 20-minute brisk walks after work, two short home sessions per week with body-weight exercises (squats, glute bridges, gentle core work), and small mobility breaks during the workday.
Within 6–8 weeks, they reported feeling noticeably better: less back stiffness, more energy, and even sleeping more soundly. By gradually working up to ~150–180 minutes of weekly moderate activity + two strength sessions per week, they hit the recommended activity levels — and felt the health benefit.
This just shows: you don’t need to become a marathon runner to feel the difference. Starting small and building up works — especially when you’re guided and supported.
How to Get Started (or Get Back on Track)
- Do a quick “activity audit”: how much are you currently moving during a typical week?
- If you’re doing nothing (or very little), set a small, achievable goal — e.g. a 10–15 min walk each day.
- Add muscle-strengthening or mobility exercises twice per week — bodyweight exercises at home are perfect.
- Sprinkle in activity throughout your day: stand or walk when you can; use the stairs; walk to shops; get off the bus early.
- Gradually increase time or intensity only when it feels comfortable — consistency is more important than intensity to start.
If you’ve got aches, pains or pre-existing issues — or haven’t exercised in ages — consider chatting to a physiotherapist (like us) to build a plan that’s safe, effective and sustainable.

Bring It All Together — Your Weekly “Movement Plan”
- Aerobic (moderate): ~150–300 minutes a week (start with 150 if you’re new)
- Or Aerobic (vigorous): ~75–150 minutes per week, if you prefer shorter, harder sessions
- Muscle strength & mobility: at least 2 days per week
- Sit less, move more: break up sedentary time during the day
Do that — and you’ll be doing what’s recommended for most Aussie adults.
FAQs
Q: What if I don’t have time for full 30-minute sessions — does short walking still count?
A: Yes — any movement helps. Even short walks, stair climbs or household chores throughout the day add up. Consistency is the main goal.
Q: Can I combine vigorous and moderate activity in the same week?
A: Definitely. The guidelines allow an equivalent combination — e.g. some brisk walking, some jogging — so you get flexibility to suit your schedule and fitness.
Q: Is strength training really necessary if I already walk or run weekly?
A: Yes — strengthening muscles supports joints, posture, mobility, and overall long-term health (especially as we age).
Q: I have a desk job. Is walking only at the weekend enough?
A: Ideally no — regular daily activity is better. Try breaking up sitting time at work, walk during breaks, and aim for smaller doses of activity most days rather than one big burst at the weekend.
Q: What if I’m older than 65 — how much should I exercise?
A: Older adults benefit from at least 30 minutes of moderate activity most days, plus strength/balance exercises — but even small amounts help.
Want a Personalised Plan?
At our clinic in Frenchs Forest we love helping people build realistic, effective movement routines. Send us a message, or give us a call today on 9806 3077 — or book online, just CLICK HERE 👈

References & Further Reading
- Australian Government: Physical activity and exercise guidelines for all Australians Health, Disability and Ageing+1
- NSW Government — Physical activity guidelines for adults NSW Government+1
- Heart Foundation — Getting started with more physical activity Heart Foundation+1
Lower back arthritis can make mornings feel like a battle before the day even begins. The good news? Physiotherapy offers targeted relief that actually improves stiffness, eases pain, and helps you move more freely. In this blog, we’ll break down what works, why it works, and how to start feeling better — starting today.

Lower Back Arthritis: Why It Happens and Why It Hurts More in the Morning
Lower back arthritis — often called lumbar osteoarthritis or facet joint arthritis — is incredibly common, especially once you hit your 40s and beyond. It happens when the joints in your lower spine become irritated or worn over time. While this sounds worrying, it’s actually very manageable when treated well.
Morning pain is one of the biggest complaints. Why? Because overnight, the joints stiffen, the muscles tighten, and inflammation settles in. So when you get out of bed, it feels like your back is stuck in “first gear” until things warm up.
If this sounds like you, you’re absolutely not alone. The key is understanding that pain doesn’t mean your back is “crumbling” — it’s simply a sign that the joints, muscles, and supporting tissues need better movement, strength, and circulation. That’s exactly where physiotherapy comes in.
How Physiotherapy Helps Lower Back Arthritis
Physiotherapy is one of the most effective, evidence-based treatments for lower back arthritis. It works by targeting the actual drivers of stiffness and pain — joint mobility, muscle tightness, inflammation, strength deficits, and movement habits.
Here’s how physio helps restore comfort and confidence in your back.

1. Improving Joint Mobility (So You Feel Less Stiff)
Facet joints — the small joints on each side of the spine — become stiff when arthritis is present. Manual therapy techniques such as joint mobilisation can gently restore movement to these joints, helping them glide more effectively.
Better joint movement = less morning stiffness, less catching, and smoother bending or twisting.
2. Reducing Muscle Tension and Spasm
When joints become irritated, the surrounding muscles jump in to “guard” the area. This is why you may feel:
- tightness around the lower spine
- aching in the buttocks
- spasms after standing for a while
- difficulty straightening up
Physiotherapy techniques such as soft-tissue release, dry needling, and stretching help switch these muscles off, reducing pressure on irritated joints.
3. Building Strength in the Right Areas
Contrary to popular belief, arthritis does not mean you should stop moving. In fact, targeted strengthening creates more support around the lower back, reducing load on the arthritic joints.
Physios focus on strengthening:
- deep core muscles
- glutes
- hip stabilisers
- lumbar extensor muscles
When these muscles work properly, the spine becomes more stable and moves with far less irritation.

4. Improving Flexibility in the Hips and Pelvis
If your hips are stiff, your lower back ends up doing extra work — and arthritic joints don’t like that.
Your physio will help restore movement in the:
- hip flexors
- hamstrings
- glute muscles
- hip capsule
Better hip mobility = less strain on the back = fewer flare-ups.
5. Correcting Posture and Movement Habits
Lower back arthritis doesn’t only flare up from “big” movements. Often, it’s the little things done poorly over and over — sitting posture, lifting technique, standing habits, or bending patterns.
A physio can analyse how you move and help correct small issues that make a huge difference long term.
6. Reducing Inflammation and Improving Circulation
Modalities such as gentle heat therapy, shockwave (in suitable cases), and exercise-based rehabilitation help improve blood flow and settle inflammation. This is particularly helpful during morning stiffness or after long days on your feet.
7. Building a Long-Term Management Plan
Perhaps the most important part of physio for lower back arthritis is education and planning.
Understanding:
- what aggravates arthritis
- what calms it
- which movements are safe
- how to maintain mobility long term
…makes all the difference in staying pain-free and active.
Common Symptoms We See in the Clinic
People with lower back arthritis often experience:
- morning stiffness lasting 30–60 minutes
- pain when standing up after sitting
- soreness with prolonged standing or walking
- aching across the lower back
- tightness in the buttocks
- difficulty bending or twisting
- “grinding” sensations or stiffness during movement
- pain relief after warming up or stretching
If this describes your daily routine, there’s a very good chance physio will help.

A Recent Patient Example (From a Surrounding Suburb)
We recently saw Sarah, a 57-year-old patient from Davidson, who came in with long-standing lower back arthritis. She was waking every morning with severe stiffness and found it hard to straighten up when getting out of the car.
At her first appointment, her lower back mobility was limited and her hip strength was low, which meant her spine was carrying more load than it should.
Over six weeks, we used:
- gentle spinal mobilisation
- hip and glute strengthening
- daily mobility drills
- a personalised morning routine to reduce stiffness
- ergonomic recommendations for working from home
By week four, she reported her morning stiffness had halved. By week six, she was walking daily without pain and didn’t feel “locked up” in the mornings anymore. She’s now maintaining progress with a simple home program.
Stories like this are incredibly common — the right treatment makes a huge difference.
What a Physiotherapy Treatment Plan Looks Like
Your plan will always be personalised, but typically includes:
Week 1–2
- Reduce muscle tension
- Improve mobility
- Calm inflammation
- Light activation exercises
- Build confidence with movement
Week 3–6
- Deeper strengthening
- Hip and glute loading
- Posture + movement retraining
- Progression of mobility techniques
Week 6+
- Long-term strength plan
- Return to walking, gym, sport, gardening
- Flare-up prevention strategies
Most people start feeling noticeably better within 2–4 weeks.
Is Lower Back Arthritis Permanent?
Arthritis itself doesn’t reverse, but your symptoms absolutely can. Pain, stiffness, and movement limitations often improve dramatically with the right approach.
Physiotherapy helps you build a body that supports your spine rather than aggravating it — that’s why so many people feel better long term.
Top Exercises for Lower Back Arthritis (Safe + Effective)
(Note: These should always be prescribed by a physio for best results.)
1. Cat–Camel Mobilisation
Gently warms up the spine and reduces morning stiffness.
2. Hip Flexor Stretch
Takes pressure off the lower back during standing and walking.
3. Glute Bridge
Strengthens the glutes and supports the lumbar spine.
4. Child’s Pose With Side Reach
Releases tightness around the lower back and sides.
5. Seated Lumbar Rotation
Improves facet joint mobility.
These exercises are incredibly effective when combined with hands-on treatment.

When to Seek Physiotherapy for Lower Back Arthritis
You should book in if you:
- feel stiff every morning
- get pain when standing after sitting
- have ongoing back pain for more than 2–3 weeks
- find movement becoming more restricted
- notice flare-ups more frequently
- feel nervous or unsure about what movements are safe
Getting on top of symptoms early prevents flare-ups and supports long-term spinal health.
FAQs
1. Can physiotherapy actually help lower back arthritis?
Yes. Physiotherapy is one of the most effective treatments for lower back arthritis. It reduces stiffness, improves mobility, strengthens the supporting muscles, and helps you manage symptoms long term.
2. Will arthritis in my lower back keep getting worse?
Arthritis naturally progresses very slowly, but symptoms do not have to get worse. With proper treatment and strengthening, most people maintain or improve comfort over time.
3. Is exercise safe if I have lower back arthritis?
Absolutely — exercise is essential. The key is choosing the right exercises that strengthen without irritating the joints. A physio can guide you through this safely.
4. Why is my lower back more painful in the morning?
When you sleep, joints stiffen and inflammation settles. This makes movement uncomfortable at first, but physiotherapy helps reduce this morning stiffness significantly.
5. How long until I notice improvements?
Most people start feeling better within 2–4 weeks, with the biggest changes seen over 6–8 weeks of consistent treatment.
References
- https://www.arthritis.org/diseases/back-pain
- https://www.healthdirect.gov.au/arthritis
- https://xphysio.com.au/blog
{
“@context”: “https://schema.org”,
“@type”: “FAQPage”,
“mainEntity”: [
{
“@type”: “Question”,
“name”: “Can physiotherapy actually help lower back arthritis?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Yes. Physiotherapy is one of the most effective treatments for lower back arthritis. It reduces stiffness, improves mobility, strengthens the supporting muscles, and helps you manage symptoms long term.”
}
},
{
“@type”: “Question”,
“name”: “Will arthritis in my lower back keep getting worse?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Arthritis naturally progresses very slowly, but symptoms do not have to get worse. With proper treatment and strengthening, most people maintain or improve comfort over time.”
}
},
{
“@type”: “Question”,
“name”: “Is exercise safe if I have lower back arthritis?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Absolutely — exercise is essential. The key is choosing the right exercises that strengthen without irritating the joints. A physiotherapist can guide you safely.”
}
},
{
“@type”: “Question”,
“name”: “Why is my lower back more painful in the morning?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “When you sleep, joints stiffen and inflammation settles. This makes movement uncomfortable at first, but physiotherapy helps reduce morning stiffness significantly.”
}
},
{
“@type”: “Question”,
“name”: “How long until I notice improvements?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Most people start feeling better within 2–4 weeks, with the biggest improvements seen over 6–8 weeks of consistent physiotherapy treatment.”
}
}
]
}
Rib pain can make simple things like breathing, laughing or rolling in bed feel impossible. The good news? Physiotherapy offers fast, effective relief for rib strains, intercostal muscle injuries and joint stiffness. In this blog, we’ll break down what causes rib pain and what physio can do to help you breathe, move and sleep more comfortably again.
Rib Pain Physiology 101: Why It Hurts So Much
Rib pain is one of those injuries that seems minor—until you get it. Because your ribs move every time you breathe, they’re constantly under load. That means that even small strains or joint irritations can flare up quickly.
Common sources of rib pain include:
- Intercostal muscle strain (the small muscles between your ribs)
- Costovertebral joint irritation (where ribs meet the spine)
- Costochondral joint inflammation (the rib cartilage at the front)
- Thoracic spine stiffness referring pain into the ribs
- Sudden twisting injuries (sport, lifting, awkward movements)
- Prolonged or forceful coughing
While rib fractures do happen, the majority of acute rib pain we see in clinic is from strain, overload or joint dysfunction, not breaks.

Why Rib Pain Takes So Long to Ease Without Help
Ribs move with:
- Every breath
- Any trunk rotation
- Reaching overhead
- Sneezing or coughing
- Lying on your side
- Rolling in bed
When irritated structures don’t get a chance to settle, rib pain can linger for weeks or months if left untreated. Physiotherapy helps break this cycle quickly by restoring normal rib mechanics, reducing muscle guarding and improving mobility in the mid-back.
How Physiotherapy Helps Rib Pain Settle Faster
1. Reduce Guarding and Muscle Spasm
After a twist or strain, the intercostal muscles tighten up to protect the area. You might feel sharp pain when inhaling deeply or turning your torso.
Physio treatment can include:
- Gentle soft tissue release
- Trigger point therapy
- Dry needling
- Heat therapy
- Rhythmic breathing techniques
This helps settle protective spasm and restores smoother rib movement.

2. Mobilise the Thoracic Spine
A stiff thoracic spine is one of the biggest contributors to rib pain. If those joints can’t move properly, the rib joints compensate—and that’s when they flare.
Your physiotherapist may use:
- Manual joint mobilisations
- Gentle manipulations
- Assisted stretching
- Postural correction
Restoring mobility reduces loading on the ribs instantly.
3. Improve Rib Position and Mechanics
Sometimes a rib becomes “stuck” in a slightly elevated or depressed position after a twist or sudden movement. This can cause:
- Sharp pain on inhalation
- Pain wrapping around the chest
- Pain with rotation
- Pain when lying on the affected side
Physios use specific rib mobilisations to restore the normal glide of the rib head and cartilage.
4. Strengthen Intercostal and Trunk Muscles
Once pain settles, strengthening helps prevent the injury from returning.
Exercises include:
- Controlled deep breathing with rib expansion
- Side bending and thoracic rotation
- Postural stability exercises
- Pilates-style trunk training
It’s all about building resilience in the rib cage so everyday movements feel natural again.
5. Support Healing After a Coughing Episode
Rib pain from coughing (especially during flu season) is a common presentation.
Physio helps by:
- Reducing spasm
- Improving breathing mechanics
- Taping to support the rib cage
- Giving cough-friendly postures
- Strengthening once the illness settles
Many people feel relief within the first few sessions.
A Real Patient Story (From a Nearby Suburb)
A few weeks ago, we treated Sarah, a 34-year-old from Belrose who strained her ribs while twisting quickly to lift her toddler out of the car. She described a sharp pain with breathing, sneezing and turning in bed.
During her assessment, we found:
- An intercostal strain
- A stiff thoracic spine
- A tender costotransverse joint
Over three sessions, we used rib mobilisations, soft tissue release, breathing retraining and gentle strengthening. By week two, Sarah could breathe deeply, sleep on her side and return to the gym pain-free.
This kind of recovery timeline is very typical when rib pain is treated early with targeted physiotherapy.
How Long Does Rib Pain Take to Heal?
Most mild strains settle within:
- 2–4 weeks with physiotherapy
- 6–8+ weeks if left untreated
Joint-related rib pain often improves even faster—sometimes within a few days with the right treatment.
Can I Exercise With Rib Pain?
Yes—but it needs to be modified.
Safe exercises early on include:
- Walking
- Gentle thoracic rotations
- Soft mobility work
- Supported deep breathing
Avoid early on:
- Heavy lifting
- Overhead movements
- Rapid twisting
- High-intensity workouts
Your physio will guide you based on your specific injury.

Hands-On Physiotherapy Treatments That Help Rib Pain
Here’s what your treatment might include:
- Soft tissue release
- Trigger point therapy
- Dry needling
- Thoracic and rib mobilisations
- Cupping (optional)
- Kinesiology taping
- Postural correction
- Guided breathing drills
- Strengthening exercises
Treatment is gentle and always tailored to your comfort levels.
The Role of Breathing Retraining
Many people with rib pain unknowingly develop shallow breathing patterns.
Your physio will teach you:
- Diaphragmatic breathing
- Lateral rib expansion
- Breathing with less upper-rib stress
- Relaxed exhalation techniques
These help:
- Reduce pain
- Improve mobility
- Reduce anxiety around breathing
It also speeds up recovery significantly.

When Should You See a Physiotherapist Immediately?
Seek professional help ASAP if you have:
- Pain that gets worse across days
- Pain that wraps around to the chest/sternum
- Difficulty sleeping due to sharp pain
- Pain with deep breathing
- A recent coughing illness
- A twisting or lifting injury
- Recurrent rib pain episodes
Early treatment prevents the body from locking up and forming long-lasting compensations.
FAQs – Rib Pain Physiotherapy
1. Is rib pain dangerous?
Most rib pain is musculoskeletal and not dangerous, but you should always get it checked if the pain is severe, spreading to your chest, or accompanied by breathing difficulty.
2. How do I know if it’s a rib strain or a fracture?
Strains usually hurt with movement and deep breathing. Fractures are more constant and sharper. Physios can assess and refer for imaging if needed.
3. Can physio fix rib joints that feel “stuck”?
Yes—rib mobilisations are one of the most effective forms of treatment.
4. Does massage help rib pain?
Absolutely. Releasing intercostal, thoracic and paraspinal muscles can reduce pain quickly.
5. How many physio sessions will I need?
Most people need 2–5 sessions, depending on the severity of the strain.
References
- https://www.physio-pedia.com/Intercostal_Muscle_Strain
- https://www.ncbi.nlm.nih.gov/books/NBK541008/
- https://xphysio.com.au/blog
{
“@context”: “https://schema.org”,
“@type”: “FAQPage”,
“mainEntity”: [
{
“@type”: “Question”,
“name”: “Is rib pain dangerous?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Most rib pain is musculoskeletal and not dangerous, but you should get it checked if the pain is severe, spreading to your chest, or accompanied by breathing difficulty.”
}
},
{
“@type”: “Question”,
“name”: “How do I know if it’s a rib strain or a fracture?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Rib strains usually hurt with movement and deep breathing. Fractures tend to feel sharper and more constant. A physiotherapist can assess and refer for imaging if needed.”
}
},
{
“@type”: “Question”,
“name”: “Can physio fix rib joints that feel stuck?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Yes. Physiotherapy rib mobilisations are highly effective at restoring normal joint mechanics and reducing pain.”
}
},
{
“@type”: “Question”,
“name”: “Does massage help rib pain?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Yes. Massage and soft tissue release reduce muscle tightness around the ribs, helping ease pain and improve mobility.”
}
},
{
“@type”: “Question”,
“name”: “How many physio sessions will I need?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Most people recover in 2–5 sessions depending on the severity and cause of their rib pain.”
}
}
]
}
Thoracic spine stiffness can sneak up on you—often starting as mild tightness before turning into frustrating aches that limit your day. The good news? Physiotherapy is one of the most effective ways to restore mid-back mobility. In this blog, we’ll break down why it happens, how physio helps, and what you can do today to move better and feel better.
Feeling “Stuck” in the Mid-Back? You’re Not Alone.
If you’ve ever tried to twist, reach, or take a deep breath and felt like your mid-back just wouldn’t budge, you’re experiencing thoracic stiffness—a problem we see in the clinic every single day.
And here’s the hook:
Your thoracic spine isn’t just about your back. When it tightens up, it affects your neck, shoulders, ribs, breathing mechanics, and even how your lower back feels.
Most people don’t realise how much this section of the spine does until it stops doing its job.
At X Physio, we help people unlock their mid-back movement using proven assessment techniques, hands-on therapy, and targeted exercises designed to build long-lasting strength and mobility. If your back feels like it’s turned into a plank of wood—this blog is for you.

What Exactly Is the Thoracic Spine?
The thoracic spine is the middle section of your back—the part that anchors your rib cage. It’s built for stability, rotation, and controlled movement. Unlike the lower back (lumbar spine), which is designed for bending and lifting, the thoracic spine is all about rotation, extension, and helping your body move efficiently as a whole.
When it becomes stiff, you start to compensate elsewhere—usually in the neck or lower back—which is how many people develop secondary pain patterns.

Common Causes of Thoracic Spine Stiffness
Thoracic stiffness rarely comes from one single thing. Instead, it’s usually a combination of lifestyle and movement habits that accumulate over time.
Here are the most common causes we see in the clinic:
1. Poor posture and prolonged sitting
Hours working on a laptop, driving, or scrolling on your phone all push the thoracic spine into flexion (rounding). Over time, your mid-back becomes “locked” in that shape.
2. Weak postural muscles
The muscles between the shoulder blades (rhomboids, mid-traps, lower traps) often become under-used. When they’re not doing their job, the spine stiffens up.
3. Limited rib mobility
Your ribs attach directly to your thoracic spine. When rib mobility drops, your thoracic rotation and extension drop too.
4. Stress and shallow breathing
Many people don’t realise that stress changes breathing mechanics. Shallow upper-chest breathing reduces rib expansion, which leads to stiffness through the mid-back.
5. Heavy training without enough mobility work
Overhead lifting, bench pressing, and rowing all rely on good thoracic movement. Without that mobility, the joints become overloaded.
6. Previous injuries
Shoulder injuries, whiplash, lower back pain, and rib injuries commonly lead to mid-back compensation patterns.

Symptoms of Thoracic Spine Stiffness
Thoracic stiffness isn’t always obvious. Sometimes it shows up in places you wouldn’t expect.
Common symptoms include:
- A tight, “blocked” sensation in the mid-back
- Difficulty taking a full breath
- Pain between the shoulder blades
- Neck tightness from over-working
- Shoulder pain during overhead movements
- Clicking or cracking in the back when stretching
- Slouching posture that feels hard to correct
- Lower back strain due to compensation
If any of these sound familiar, thoracic spine physiotherapy may be exactly what you need.

How Physiotherapy Helps Thoracic Stiffness
Effective physiotherapy treatment for thoracic stiffness includes several key components. We don’t just crack your back and send you off—we fix the root cause and teach you how to maintain mobility long-term.
Here’s what a typical physio treatment plan looks like at X Physio:
1. Thorough Assessment
We start by identifying the specific areas that are stiff, weak, or overloaded. This may include:
- Thoracic joint mobility testing
- Rib cage and breathing assessment
- Posture analysis (sitting, standing, lifting)
- Shoulder and neck mobility
- Functional movements like rotation, reaching, lifting
The aim is simple: find out why your thoracic spine is stiff—then build the right plan to address it.
2. Hands-On Manual Therapy
This is one of the quickest ways to improve mid-back mobility. Treatment may include:
- Thoracic joint mobilisations
- Thoracic extension and rotation mobilisation
- Soft tissue release around the spine
- Rib mobilisations
- Dry needling (when appropriate)
Patients are often surprised at how much better they feel immediately after hands-on therapy.
This creates the “window of opportunity” where exercises work even better.

3. Mobility Exercises to Restore Movement
We prescribe targeted mobility drills that match your stiffness pattern.
These may include:
- Cat-camel variations
- Open book rotations
- Foam roller thoracic extensions
- Quadruped rotations
- Chair-based extension exercises
These drills help retrain your spine to move the way it’s supposed to.

4. Strength Training for Long-Term Change
Mobilising the spine is only half the story. Strengthening the muscles that support good posture and movement makes the improvements stick.
We may include:
- Scapular retraction and depression work
- Lower trap strengthening
- Thoracic extensor strengthening
- Functional rotation training
- Rowing variations
- Overhead movement retraining
Once your thoracic spine learns to move and your postural muscles become stronger, stiffness becomes far less likely to return.
5. Breath Retraining
This is often the missing piece of the puzzle.
Deep diaphragmatic breathing restores rib mobility and reduces mid-back compression.
We use:
- 360-degree rib expansion drills
- Breath-led thoracic rotation
- Breathing coordination for posture
Restoring normal breathing patterns can dramatically reduce thoracic rigidity.

6. Education & Habit Changes
We help you understand:
- How to sit without loading your spine
- How to train safely during rehab
- What activities to avoid temporarily
- How to stretch at work
- How to prevent the stiffness returning
Our goal is to empower you with long-term solutions—not keep you coming back forever.
Real Patient Example — From Beacon Hill, NSW
Recently, we treated Sarah, a 38-year-old office worker from Beacon Hill, a surrounding suburb of Frenchs Forest. She came in with constant mid-back tightness and shoulder discomfort that had been slowly getting worse over six months.
Her assessment showed:
- Very limited thoracic extension
- Weak mid-back postural muscles
- Poor rib mobility
- Compensation through the neck and lower back
After four weeks of thoracic spine physiotherapy—including hands-on mobilisation, breath retraining, mobility drills, and postural strengthening—she reported:
- Significant reduction in stiffness
- Improved posture without forcing it
- Better overhead shoulder mobility
- Easier deep breathing
- No more “tight block” sensation at work
Her progress is a perfect example of how targeted thoracic physiotherapy can restore movement and eliminate pain quickly.
Best Exercises for Thoracic Spine Stiffness
Here are some of our favourite go-to exercises:
1. Foam Roller Thoracic Extension
Great for reversing hours of slouching and opening up the chest.
2. Open Book Rotations
Excellent for improving rotation and easing rib tightness.
3. Quadruped Thread-the-Needle
Fantastic for freeing up the upper and mid-back.
4. Wall Angels
Builds strength, mobility, and postural awareness.
5. Seated or Kneeling Thoracic Extension
A practical exercise you can even do at the office.
6. Rowing Variations
Strengthens the muscles that keep your thoracic spine mobile.
We tailor these (and more) to your specific stiffness pattern.

When to See a Physiotherapist
Thoracic stiffness is extremely common—but it isn’t something you need to put up with. You should consider seeing a physio if:
- The tightness isn’t improving
- Stretching helps only temporarily
- You’re getting shoulder, neck, or rib pain as well
- Breathing feels restricted
- Pain worsens with work or exercise
- You’re relying on cracking your back for relief
If your stiffness is impacting daily life, early physiotherapy makes a massive difference.
References
- https://www.physio-pedia.com/Thoracic_Spine
- https://www.healthdirect.gov.au/back-pain
- https://xphysio.com.au/blog
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3106778/
FAQs – Thoracic Spine Physiotherapy
1. What causes thoracic spine stiffness?
Thoracic stiffness is usually caused by poor posture, prolonged sitting, stress, muscle weakness, limited rib mobility, and lack of rotation or extension in daily movement.
2. Can physiotherapy actually improve thoracic mobility?
Yes. Physiotherapy uses joint mobilisation, hands-on release, mobility drills, strength work, and breath retraining to restore normal movement through the mid-back.
3. How long does it take to feel better?
Most people feel an improvement within 1–2 sessions, with more lasting changes over 3–6 weeks depending on the severity.
4. Can thoracic stiffness cause neck or shoulder pain?
Absolutely. The thoracic spine forms the foundation of upper-body movement. If it’s stiff, the neck and shoulders start compensating, often leading to pain.
5. What exercises help with thoracic tightness?
Foam roller extensions, open books, wall angels, and thread-the-needle variations are some of the most effective exercises.
{
“@context”: “https://schema.org”,
“@type”: “FAQPage”,
“mainEntity”: [
{
“@type”: “Question”,
“name”: “What causes thoracic spine stiffness?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Thoracic stiffness is usually caused by prolonged sitting, posture habits, weak postural muscles, limited rib mobility, and reduced rotation or extension through the mid-back.”
}
},
{
“@type”: “Question”,
“name”: “Can physiotherapy actually improve thoracic mobility?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Yes. Physiotherapy restores thoracic mobility through joint mobilisation, soft tissue release, rib mobility work, mobility drills, postural strengthening, and breathing retraining.”
}
},
{
“@type”: “Question”,
“name”: “How long does it take to feel better?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Many people feel better within 1–2 sessions, with long-term improvements typically achieved over 3–6 weeks depending on the severity.”
}
},
{
“@type”: “Question”,
“name”: “Can thoracic stiffness cause neck or shoulder pain?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Yes. The thoracic spine influences how the neck and shoulders move. If it’s stiff, these areas can overwork and become painful.”
}
},
{
“@type”: “Question”,
“name”: “What exercises help with thoracic tightness?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Foam roller extensions, open book rotations, thread-the-needle, wall angels, and thoracic extension drills are among the most effective exercises.”
}
}
]
}
Gluteal tendinopathy can make simple things like sitting at work or sleeping on your side feel impossible. Physiotherapy is one of the most effective ways to reduce pain, rebuild strength and get you comfortable again. In this blog, we’ll break down exactly how physio helps, plus practical tips you can start today—so keep reading.
Physio for Gluteal Tendinopathy: Sitting and Sleeping Without Pain
Gluteal tendinopathy is one of the most frustrating conditions we see in clinic. It’s sneaky, annoying and usually flares up during everyday things—sitting too long, crossing your legs, walking uphill, or simply lying in bed at night. Some people even say it feels like “a deep ache that never switches off.”
The good news? Gluteal tendinopathy physiotherapy works exceptionally well when it’s targeted, progressive and tailored to how your hip actually behaves.
Today, we’ll walk through:
- what gluteal tendinopathy actually is
- why sitting and sleeping are often the worst triggers
- how physiotherapy reduces pain and rebuilds tendon strength
- the modifications that make life easier right away
- a real patient success story from a nearby Northern Beaches suburb
- FAQs with schema markup you can paste directly into WordPress
Let’s dive in.

What Is Gluteal Tendinopathy?
Gluteal tendinopathy is irritation or overload of the tendons on the side of your hip—mainly the gluteus medius and gluteus minimus tendons. These tendons help stabilise your hip and pelvis when you walk, climb stairs, or stand on one leg.
When these tendons are overloaded (gradually or suddenly), they become sensitive and less tolerant to compression or stretch. This is why many people feel pain when:
- lying on their side
- crossing their legs
- sitting for long periods
- bending the hip too much
- walking on uneven ground or hills
It’s extremely common in women aged 40+ but can affect anyone—especially office workers, runners and active adults.

Why Sitting Hurts With Gluteal Tendinopathy
It seems counterintuitive—sitting is meant to be restful, right? Unfortunately, not for this condition.
When you sit, the tendons on the outside of the hip are pulled into a slightly stretched and compressed position. This is especially true if you:
- sit with your legs crossed
- sit with your knees together
- sit on a soft couch where your hips drop into one side
- sit for hours without moving
Over time, this compressive force irritates the tendon even more.
Quick Sitting Fixes You Can Use Today
- Sit with your feet hip-width apart
- Keep knees apart (not touching)
- Use a firmer chair at work
- Add a small pillow under your thigh (not hip)
- Stand up every 20–40 minutes
Small changes = big relief.

Why Sleeping Flare-Ups Are So Common
One of the classic gluteal tendinopathy complaints is:
“I can’t sleep on my side anymore—it aches like mad.”
When lying on your side, the top leg can drop across the body, dragging the tendon into a stretched and compressed position. The bottom hip can also get irritated by direct pressure from the mattress.
Sleeping Adjustments That Help Immediately
If lying on your side:
- Place a thick pillow between your knees to keep the top hip neutral
- Hug a pillow to prevent rolling forward
- Use a mattress topper if the bottom hip is too compressed
If lying on your back:
- Place a pillow under your knees to reduce hip tension
None of these solve the problem—but they reduce irritation while we rebuild tendon tolerance through physiotherapy.
How Physiotherapy Treats Gluteal Tendinopathy
Effective gluteal tendinopathy physiotherapy doesn’t just treat the painful area. It involves reducing load temporarily, correcting irritants, and gradually building the tendon’s capacity.
Here’s what the best evidence-based approach looks like.
1. Reducing Tendon Compression (The First Priority)
Your physio will identify which movements or positions are compressing the tendon. These are commonly:
- side sleeping
- sitting with legs crossed
- leaning on one hip
- over-striding during walking
- excessive stretching of the glutes
You don’t need to avoid everything forever—just while the tendon is calming down. This phase is about creating a safe environment for healing.

2. Strengthening the Gluteal Tendons in the Right Way
Not all exercises are helpful. Some make things worse.
Good gluteal strengthening is progressive, controlled, and non-compressive early on. Examples include:
- isometric hip abduction holds
- bridge variations
- side-lying hip abduction with careful technique
- standing hip hitching
- later: resistance band abduction, step-downs, controlled single-leg work
The aim is to gradually increase the tendon’s load tolerance without aggravation.

3. Improving Pelvic Control and Movement Patterns
Many people unknowingly move in ways that increase tendon strain, such as:
- dropping the hip when standing on one leg
- poor trunk control
- walking with excessive hip sway
- gripping through the outer hip muscles
Your physio helps refine technique so that daily tasks place less stress on the tendon.
4. Modifying Walking, Running and Training (If Needed)
A physio may adjust:
- stride length
- pace
- inclines
- running cadence
- gym exercises that could be irritating
This isn’t about stopping activity—it’s about doing it safely.
5. Hands-On Treatment for Pain Relief
Soft tissue release, massage and gentle joint mobilisations can reduce irritation and pain. While hands-on therapy won’t fix the tendon alone, it supports the strengthening program so you progress faster.
6. Shockwave Therapy (If Required)
Shockwave can help stubborn gluteal tendinopathy by stimulating local blood flow and reducing sensitivity. Your physio may recommend it if symptoms haven’t improved after a few weeks of strengthening.
A Real Patient Story From Our Clinic
Recently, we saw a patient from Belrose, just a short drive from our clinic in Frenchs Forest. She’d been struggling with hip pain for over a year—particularly when sitting at work and every night when trying to sleep on her side.
She’d tried stretching, foam rolling and even a new mattress, but nothing helped.
During her physiotherapy assessment, we found:
- significant tenderness over the gluteus medius tendon
- reduced single-leg control
- aggravation when crossing her legs
- poor side-sleeping alignment
- weak hip abduction strength
We started her on a structured strengthening program, adjusted her workspace setup, and gave her simple sleeping modifications. Within two weeks, she could sit comfortably at work again. Within six weeks, her night pain had almost completely resolved. She’s now back to walking trails on the weekends—pain-free.
Stories like this are extremely common. With the right approach, gluteal tendinopathy responds beautifully to physiotherapy.
Everyday Tips to Reduce Pain Immediately
Here are practical things you can start today:
Avoid:
- Sitting cross-legged
- Deep glute stretches
- Side sleeping without support
- Standing with your hip “popped out”
- Long hill walks early in rehab
Do More Of:
- Short movement breaks at work
- Side sleeping with a pillow between knees
- Controlled strengthening exercises
- Firm chair sitting
- Keeping knees apart
These reduce irritation so your tendon can actually heal.
Long-Term Outlook: How Long Until It Gets Better?
Most people see significant improvement within:
- 4–6 weeks → reduced pain
- 8–12 weeks → stronger tendon and improved movement
- 3–6 months → full return to normal activity
Tendons take time to adapt, but with consistency, the results can be life-changing.
When Should You See a Physio?
Book an appointment if you’re experiencing:
- pain on the outside of your hip
- discomfort when sitting or sleeping
- limping first thing in the morning
- pain climbing stairs or hills
- tenderness on the bony part of your hip
- clicking, catching or a feeling of weakness
The earlier you start treatment, the quicker your recovery.

Conclusion
Gluteal tendinopathy doesn’t have to control your sitting, sleeping or movement. Physiotherapy is a proven, effective and long-lasting solution that helps you reduce pain, build strength and get back to the activities you enjoy.
If your hip has been bothering you for weeks (or months), now’s the perfect time to get it sorted.
Give us a call today on 9806 3077, or book online, just CLICK HERE.
References
- https://completephysiotherapy.co.uk
- https://choose.physio
- https://xphysio.com.au/blog
- https://www.physio-pedia.com/Gluteal_Tendinopathy
- https://www.healthdirect.gov.au
FAQs
1. What is gluteal tendinopathy?
Gluteal tendinopathy is irritation of the gluteus medius or minimus tendons on the outside of the hip, causing pain with sitting, sleeping, walking or climbing stairs.
2. How does physiotherapy help?
Physio reduces tendon irritation, rebuilds strength, improves hip control and helps you avoid common triggers so the tendon can recover properly.
3. Why does it hurt to sleep on my side?
Side sleeping compresses and stretches the irritated tendon. A pillow between your knees helps reduce this strain.
4. Should I stretch my hip?
Deep glute stretches often make symptoms worse. Strengthening is far more effective for tendon recovery.
5. How long until it gets better?
Most people notice improvement within 4–6 weeks, with full recovery taking 8–12 weeks or longer depending on severity.
{
“@context”: “https://schema.org”,
“@type”: “FAQPage”,
“mainEntity”: [
{
“@type”: “Question”,
“name”: “What is gluteal tendinopathy?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Gluteal tendinopathy is irritation of the gluteus medius or minimus tendons on the outside of the hip, causing pain with sitting, sleeping, walking or climbing stairs.”
}
},
{
“@type”: “Question”,
“name”: “How does physiotherapy help?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Physiotherapy reduces tendon irritation, rebuilds strength, improves hip control and helps you avoid common triggers so the tendon can recover properly.”
}
},
{
“@type”: “Question”,
“name”: “Why does it hurt to sleep on my side?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Side sleeping compresses and stretches the irritated tendon. Using a pillow between your knees helps reduce this strain.”
}
},
{
“@type”: “Question”,
“name”: “Should I stretch my hip?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Deep glute stretches often make symptoms worse. Strengthening is usually more effective for tendon recovery.”
}
},
{
“@type”: “Question”,
“name”: “How long until it gets better?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Most people notice improvement within 4–6 weeks, with full recovery taking 8–12 weeks depending on severity and consistency with physiotherapy.”
}
}
]
}
A Baker’s cyst behind the knee can feel tight, achey and downright annoying—especially when it limits bending or straightening your knee. The good news? Physiotherapy can often reduce swelling, improve movement and help the cyst settle faster. In this blog, we’ll unpack what actually works, common mistakes, and when to seek extra help.
What Is a Baker’s Cyst, and Why Does It Form?
A Baker’s cyst (also called a popliteal cyst) is a fluid-filled swelling that forms at the back of the knee. It’s not dangerous, but it can be uncomfortable—especially during walking, squatting, stairs or running.
A cyst generally develops when excess fluid from within the knee joint gets pushed into a small pocket at the back of the knee, causing bulging and pressure. Think of it like a balloon that fills up whenever your knee becomes irritated.
Common causes include:
- Knee osteoarthritis
- Meniscus irritation or tears
- Knee joint swelling after injury
- Inflammatory conditions
- Overuse from sport or repetitive bending
In many cases, the cyst isn’t the real problem—the swelling inside the knee is.
Symptoms of a Baker’s Cyst
Every patient feels it slightly differently, but the most common symptoms include:
- Tightness or fullness behind the knee
- Difficulty bending or straightening the knee fully
- A noticeable lump at the back of the knee
- Aching with walking, hills, kneeling or prolonged standing
- Stiffness in the morning
- Clicking or catching sensations
Some people describe it as “a water balloon sitting behind my knee.”
Occasionally, the cyst can leak or rupture, causing sharp calf pain and swelling—something often mistaken for a DVT (deep vein thrombosis). Physiotherapists are trained to screen for this and refer if needed.
How Physiotherapy Helps a Baker’s Cyst Settle
The truth is simple:
If you reduce the irritation inside the knee, the cyst usually shrinks or disappears on its own.
That’s why physiotherapy is such an effective treatment option—it targets the cause, not just the lump.
Here’s what a physiotherapist typically focuses on:
1. Reducing Knee Joint Swelling
Swelling inside the knee increases the pressure that pushes fluid backward into the cyst. We use:
- Manual therapy
- Gentle joint mobilisations
- Soft tissue release
- Compression
- Activity modification
- Targeted exercises to improve fluid movement
This alone often reduces cyst size significantly within a few weeks.

2. Strengthening the Muscles That Support the Knee
Weak quads, hamstrings and calves can place extra stress on the knee joint. Strengthening these muscles improves alignment and reduces irritation.
Common exercises may include:
- Quad sets
- Step-downs
- Glute strengthening
- Hamstring control drills
- Calf raises
Your physio will tailor these to where your knee is currently at.
3. Improving Knee Mobility
Stiffness (especially from arthritis or prolonged swelling) can worsen the cyst. Gentle mobility exercises help the knee pump fluid out more effectively.
This may include:
- Heel slides
- Flexion–extension mobility drills
- Tibial rotation mobility
- Joint glides
4. Taping or Bracing (Optional)
In some cases, taping techniques help reduce excessive pressure in the joint, allowing inflammation to settle.
For more irritated knees or those with arthritis, a temporary brace may also help with walking comfort.
5. Addressing Underlying Knee Issues
If the cyst is linked to:
- A meniscus tear
- Osteoarthritis “flare”
- Patellofemoral overload
- Tendon irritation
…then treating the underlying condition is essential. Otherwise the cyst will keep coming back.
Physiotherapy manages these conditions by improving load tolerance, correcting biomechanics, and modifying daily activities so the knee can recover.
6. Education and Load Management
Many people unknowingly make their cyst worse with:
- Excessive squatting
- Kneeling
- Deep lunges
- Prolonged standing
- Overtraining
Your physio will help you balance movement with rest, reduce irritating loads, and reintroduce activities safely.

Will a Baker’s Cyst Disappear With Physiotherapy?
In many cases—yes.
If the underlying cause is treated and swelling is reduced, the cyst often shrinks dramatically over a 6–12 week period. Some disappear completely.
If the cyst is large or linked to severe arthritis, it may take longer, but most people still experience significant relief and better mobility.
Occasionally, cysts persist. In those cases, options may include:
- Ultrasound-guided aspiration
- Cortisone injection
- Surgical review (rare, only for chronic and painful cases)
But for the majority, physiotherapy remains the first and most effective treatment.

A Real Example From Our Clinic
Recently, we treated a patient from a nearby suburb of Belrose, NSW, who came in with a painful Baker’s cyst that developed after an increase in bushwalking and hill training. They described a tight swelling behind their right knee, which made bending difficult and stairs uncomfortable.
After a thorough assessment, we found that the underlying issue was irritation of the medial meniscus combined with early osteoarthritis changes, causing joint swelling that pushed fluid into the cyst.
Their treatment plan involved:
- Gentle manual therapy
- Quadriceps and glute strengthening
- Swelling reduction strategies
- Activity pacing (reducing steep hill climbs temporarily)
- Improving knee mobility
Within four sessions (over three weeks), they reported significantly less tightness and swelling, and the cyst reduced to almost half its original size. By week six, they were walking hills again with minimal discomfort.
This is a great example of how treating the knee, not just the cyst, produces excellent results.
What to Expect During Physiotherapy
Your physio will:
- Assess your knee movement, strength and alignment
- Identify the underlying cause of swelling
- Check for red flags such as possible cyst rupture
- Create a personalised plan to reduce swelling and strengthen the knee
- Show you specific exercises to help the cyst settle
- Monitor your progress and adjust the plan as your knee improves
Most people notice improvement within 2–4 weeks, with full recovery taking 6–12 weeks depending on the cause.
Can You Exercise With a Baker’s Cyst?
The short answer: yes, but smartly.
Good exercises:
- Cycling (gentle)
- Swimming
- Leg strengthening
- Glute exercises
- Light walking
Exercises to avoid early on:
- Deep squats
- Heavy lunges
- Running up hills
- Kneeling
- Plyometric training
Your physio will guide you on what to keep, modify, or temporarily pause.

When To Seek Physiotherapy or Medical Help
Contact a physio or GP promptly if you experience:
- Rapid swelling
- A sudden “pop” with calf pain
- Severe heat or redness
- Difficulty weight-bearing
- Symptoms that worsen despite rest
These may indicate a ruptured cyst, infection or more complex knee issue.
FAQs
What is the fastest way to reduce a Baker’s cyst?
The quickest results usually come from reducing the swelling inside the knee through physiotherapy, targeted exercises and activity modification.
Can a Baker’s cyst burst?
Yes. If it ruptures, fluid can leak into the calf, causing pain and swelling. Physiotherapists can assess this and ensure it’s not something more serious like a DVT.
Do I need an MRI for a Baker’s cyst?
Not always. Most cysts can be diagnosed clinically. An MRI is only needed if your physio suspects a meniscus tear, cartilage injury or unexplained swelling.
How long does it take to heal?
Most people see improvement within 2–4 weeks, with full recovery often taking 6–12 weeks depending on the underlying knee issue.
Does physiotherapy actually make the cyst go away?
Yes—by reducing internal knee swelling and improving mechanics, physiotherapy often helps the cyst shrink or disappear naturally.
References
- Arthritis Australia – Knee osteoarthritis information
- Sports Medicine Australia – Knee injury management guidelines
- X Physio Blogs:
{
“@context”: “https://schema.org”,
“@type”: “FAQPage”,
“mainEntity”: [
{
“@type”: “Question”,
“name”: “What is the fastest way to reduce a Baker’s cyst?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “The quickest results usually come from reducing the swelling inside the knee through physiotherapy, targeted exercises and activity modification.”
}
},
{
“@type”: “Question”,
“name”: “Can a Baker’s cyst burst?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Yes. If it ruptures, fluid can leak into the calf, causing pain and swelling. Physiotherapists can assess this and ensure it’s not something more serious like a DVT.”
}
},
{
“@type”: “Question”,
“name”: “Do I need an MRI for a Baker’s cyst?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Not always. Most cysts can be diagnosed clinically. An MRI is only needed if your physio suspects a meniscus tear, cartilage injury or unexplained swelling.”
}
},
{
“@type”: “Question”,
“name”: “How long does it take to heal?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Most people see improvement within 2–4 weeks, with full recovery often taking 6–12 weeks depending on the underlying knee issue.”
}
},
{
“@type”: “Question”,
“name”: “Does physiotherapy actually make the cyst go away?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Yes—by reducing internal knee swelling and improving mechanics, physiotherapy often helps the cyst shrink or disappear naturally.”
}
}
]
}
Neck and shoulder pain is one of the most common issues we see in office workers—usually caused by long hours at the desk, stress, and poor posture. The good news? Physiotherapy can ease tension quickly and help prevent it from creeping back. In this blog, we’ll unpack the real causes, the best treatments, and what actually works long-term.

The Modern Office Worker Problem: Why Neck and Shoulder Pain Happens
If you work at a desk, you’ve probably felt that familiar tightness creeping up your shoulders by mid-afternoon—or the stubborn knot at the base of your neck that just never goes away. You’re not alone. Neck and shoulder pain is now a leading musculoskeletal complaint among Australians working in corporate, healthcare, education, tech and hybrid roles.
The root cause? Usually a combination of these factors:
1. Prolonged sitting
Sitting still for hours causes upper back and neck muscles to fatigue. When they tire, the smaller muscles around the neck overwork and tighten.
2. Poor desk setup
A laptop placed too low or a monitor set too far away forces your head forward, placing huge stress on the cervical spine.
3. Stress and tension
Many office workers subconsciously “shrug” their shoulders when they’re stressed, which causes the upper trapezius muscles to stay switched on all day.
4. Forward-head posture
For every 2–3cm your head moves forward, the load on the neck muscles can double. Over time, this becomes chronic pain, stiffness and even headaches.
5. Reduced movement variety
Even if you have a “perfect” ergonomic setup, staying still too long is the real enemy. Movement is what keeps the muscles happy.
The good news? Physiotherapy directly targets each of these root causes and gives you real, lasting relief.

How Physiotherapy Helps Neck and Shoulder Pain
At X Physio in Frenchs Forest, we take a structured approach to reducing pain, improving mobility, and building long-term resilience. Here’s how physio helps:
1. Hands-on treatment for immediate relief
Manual therapy is one of the fastest ways to reduce tension and restore mobility. We commonly use:
- Soft tissue release
- Trigger point therapy
- Joint mobilisation
- Dry needling (when appropriate)
These hands-on techniques reduce muscle guarding, improve circulation, and help the nervous system down-regulate its pain response.
2. Restoring movement and mobility
When the neck and shoulders stop moving well, everything stiffens up. Physiotherapy helps restore:
- Cervical rotation (turning the head)
- Thoracic extension (straightening the upper back)
- Scapular (shoulder blade) movement
- Rib mobility
Even small mobility improvements can dramatically reduce daily pain levels.
3. Strengthening the right muscles
Tight muscles are often weak muscles simply working overtime. Strengthening key areas reduces load on irritated tissues:
- Deep neck flexors
- Lower trapezius
- Serratus anterior
- Rotator cuff
- Thoracic extensors
You don’t need a gym for this—most exercises are simple, low-load movements perfect for home or the office.

4. Posture coaching (but not the outdated kind)
Posture is not about sitting “perfectly straight”—it’s about staying adaptable. We help you:
- Adjust your workstation ergonomics
- Learn micro-break strategies
- Understand what “good movement variety” looks like
- Reduce tension habits (like shrugging or clenching)
Our goal is to help you move more, not sit still in a rigid position.
5. Stress and tension management strategies
Many cases of neck and shoulder pain are linked to stress. We integrate simple, practical strategies such as:
- Breathing control
- Relaxation techniques
- Gentle mobility routines you can use between meetings
These help calm the nervous system so it stops amplifying your pain signals.
6. Preventing flare-ups
One of the strongest benefits of physiotherapy is learning how to stop pain coming back.
We work with you to:
- Identify your individual triggers
- Build strength and mobility in weak links
- Create a personalised home plan
- Gradually increase your tolerance to sitting, work and exercise
Long-term success is all about consistency—not perfection.
A Real Example: Patient Success Story from a Nearby Suburb
Recently, we treated Courtney, a 37-year-old accountant from Dee Why, who came in with persistent neck and shoulder pain that had been bothering her for almost 18 months. She worked mostly from home and noticed the pain was worst during busy periods when she barely left her desk.
She reported:
- Tightness across the top of both shoulders
- Frequent tension headaches
- A pulling sensation when she turned her head
- Pain when lifting her children into the car
- Difficulty concentrating by the afternoon
After a detailed assessment, we identified:
- Reduced cervical rotation
- Overactive upper trapezius muscles
- Weak deep neck flexors
- Limited thoracic mobility
- A poorly adjusted home office setup
Her Treatment Plan Included:
- Hands-on release to her upper traps and neck muscles
- Thoracic joint mobilisation
- Dry needling to reduce stubborn muscle guarding
- A personalised strengthening program
- A few simple ergonomic changes
- A “2-minute mobility break” routine for work days
The Result?
By the third session, her pain had reduced by 60%.
By week four, she reported her first “completely pain-free workday in over a year”.
By week six, she was confidently exercising again and hadn’t experienced another headache.
This is a typical outcome when treatment is targeted, consistent, and based on the root cause—not just the symptoms.
The Link Between Neck Pain, Shoulder Pain and Headaches
Many office workers don’t realise that their headaches are often coming from their neck. This is called cervicogenic headache, and it happens when tightened cervical muscles refer pain upwards.
Signs your headaches are neck-related include:
- Pain that starts in the neck or base of the skull
- Headaches triggered by work or sitting
- Soreness when pressing along the neck muscles
- Reduced neck movement
- Pain on one side of the head
Physiotherapy is extremely effective at treating this type of headache because it treats the source—not just the pain.
Best Exercises for Neck and Shoulder Tension
Here are a few office-friendly exercises that help reduce pain and tightness. These should be performed gently and consistently:
1. Chin tucks (deep neck flexor activation)
Strengthens the muscles that support the neck and improve alignment.
2. Scapular retraction
Helps balance the overactive shoulder muscles.
3. Thoracic extension over a rolled towel
Releases stiffness in the upper back.
4. Upper trapezius and levator scapulae stretches
Relieves the most common tension areas.
5. Shoulder external rotation strengthening
Supports shoulder blade control and reduces load on the neck.
We provide personalised exercise programs based on your specific assessment—not generic templates.

How Long Does It Take to Improve Neck and Shoulder Pain?
Most patients feel noticeably better within 2–3 sessions, especially with the right combination of hands-on treatment and tailored exercises.
Chronic cases may require 12 weeks to fully restore strength, mobility, and postural control.
The key factor in long-term success is consistency with your exercises and movement habits.
Should You See a Physiotherapist or Just Stretch?
Stretching feels good—but it rarely solves the underlying issue on its own.
If your pain:
- Keeps returning
- Affects your sleep
- Causes headaches
- Limits your movement
- Interferes with work or gym
- Has lasted more than 2 weeks
…it’s time for a proper physiotherapy assessment.
A physio can pinpoint the exact structure causing your pain and tailor your treatment properly.
When Neck and Shoulder Pain Becomes More Serious
While most cases are mechanical and easily treatable, seek assessment if you experience:
- Numbness or tingling into the arms
- Weakness in the hands
- Severe pain that appears suddenly
- Pain following an accident
- Persistent headaches or dizziness
These symptoms may indicate nerve involvement or other conditions requiring targeted care.

FAQs About Neck and Shoulder Pain (with Schema Markup Below)
1. What causes neck and shoulder pain in office workers?
Neck and shoulder pain is often caused by poor posture, prolonged sitting, muscle fatigue, stress, and reduced movement. Over time these factors overload the neck and upper back muscles, leading to stiffness and pain.
2. How can physiotherapy help with neck and shoulder tension?
Physiotherapy helps by reducing muscle tightness, restoring movement, improving posture, and strengthening the muscles that support your neck and shoulders. Treatment includes hands-on therapy, exercises, ergonomic advice and strategies to prevent recurrence.
3. How long does it take to see results from physio?
Most patients feel improvement within 1–3 sessions, depending on the severity of the issue. Chronic or long-standing pain may take several weeks to fully resolve.
4. Can office ergonomics really make a difference?
Yes. A properly set-up workstation can significantly reduce stress on your neck and shoulders. Even small adjustments to monitor height, chair support, or keyboard position can reduce tension.
5. Do I need imaging for neck and shoulder pain?
Not usually. Most office-related neck and shoulder pain is mechanical and responds well to physiotherapy without the need for scans.
References
- X Physio Blog – https://xphysio.com.au/blog/
- Australian Physiotherapy Association
- https://ergonomics.org.au/Ergonomics Australia
Ready to Fix Your Neck and Shoulder Pain?
Don’t let daily tension or office stress control your life.
Give us a call today on 9806 3077, or book online — just CLICK HERE:
https://x-physio.au4.cliniko.com/bookings#service
{
“@context”: “https://schema.org”,
“@type”: “FAQPage”,
“mainEntity”: [
{
“@type”: “Question”,
“name”: “What causes neck and shoulder pain in office workers?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Neck and shoulder pain is usually caused by poor posture, prolonged sitting, muscle fatigue, stress, and limited movement, which overload the neck and upper back muscles.”
}
},
{
“@type”: “Question”,
“name”: “How can physiotherapy help with neck and shoulder tension?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Physiotherapy helps reduce muscle tightness, restore mobility, improve posture and strengthen supporting muscles through hands-on treatment, exercises and ergonomic advice.”
}
},
{
“@type”: “Question”,
“name”: “How long does it take to see results from physio?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Most patients feel improvement within 1–3 sessions, while chronic cases may take several weeks depending on the severity and contributing factors.”
}
},
{
“@type”: “Question”,
“name”: “Can office ergonomics really make a difference?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “Yes. Correct ergonomic setup reduces strain on the neck and shoulders by improving posture and decreasing muscle fatigue.”
}
},
{
“@type”: “Question”,
“name”: “Do I need imaging for neck and shoulder pain?”,
“acceptedAnswer”: {
“@type”: “Answer”,
“text”: “In most cases, no. Office-related neck and shoulder pain typically responds well to physiotherapy without the need for scans.”
}
}
]
}
Feeling a sharp ache or burning pain on the outside of your knee after a run? You might be dealing with IT Band Syndrome — one of the most common overuse injuries in runners. The good news? With the right IT band syndrome physiotherapy, you can get back to running pain-free faster than you think. Let’s break down what causes it, how physio helps, and what a real recovery looks like.
What Is IT Band Syndrome?
The Iliotibial (IT) Band is a thick band of connective tissue that runs along the outer thigh from the hip to the knee. It plays a key role in stabilising your knee during movement, especially when running or cycling.
IT Band Syndrome (ITBS) happens when this band becomes irritated or inflamed as it rubs repeatedly against the outside of the femur near the knee. The result? Pain that starts subtly and worsens the more you train — particularly during long runs, downhill running, or after increasing your mileage too quickly.

Common Symptoms of IT Band Syndrome
Typical signs of IT band irritation include:
- Sharp or burning pain on the outside of the knee, especially after a few kilometres into your run
- Pain that worsens with downhill or repetitive knee bending
- Tenderness or a “snapping” feeling along the outer knee
- Mild swelling or tightness around the hip or thigh
- Discomfort when going up or down stairs
Left untreated, it can develop into a chronic issue, sidelining your running and daily activities for weeks or even months.

What Causes IT Band Syndrome?
Contrary to popular belief, ITBS isn’t just about “tightness.” It’s usually a result of biomechanical imbalances and training errors that cause excessive strain on the IT band.
Here are the most common causes we see at X Physio Frenchs Forest:
1. Weak Glutes and Hips
When the gluteus medius and other hip stabilisers aren’t doing their job, the IT band picks up the slack — increasing friction and irritation along the knee.
2. Poor Running Form
Over-striding, inward knee collapse (valgus), and running with excessive hip drop all contribute to increased IT band tension.
3. Sudden Training Load Increases
Jumping from 5km runs to 10km overnight, or adding extra hill sessions, can quickly overload the IT band.
4. Muscle Imbalances
Tightness in the tensor fasciae latae (TFL) and quadriceps, combined with weak hamstrings or glutes, creates a perfect storm for IT band irritation.
5. Footwear & Surface Changes
Old running shoes, hard surfaces, or constantly running on cambered roads can all change your lower limb biomechanics, leading to ITBS.

How Physiotherapy Helps IT Band Syndrome
At X Physio, our approach to IT band syndrome physiotherapy goes beyond treating symptoms. We focus on identifying why the problem started, fixing those root causes, and guiding you back to safe, pain-free running.
Here’s what your treatment may include:
1. Comprehensive Assessment
Your physiotherapist will start by assessing your:
- Running gait and biomechanics
- Hip, knee and ankle alignment
- Strength and flexibility of key muscle groups
- Training history and footwear habits
This helps pinpoint whether your IT band pain is truly ITBS or something else, such as:
- Lateral meniscus irritation
- Biceps femoris tendinopathy
- Lateral collateral ligament (LCL) strain
Correct diagnosis is key — and that’s where expert physiotherapy makes all the difference.
2. Hands-On Manual Therapy
Early treatment often includes manual techniques to reduce pain and tension, such as:
- Soft tissue release and deep massage to the TFL, glutes and IT band
- Dry needling or trigger point therapy
- Joint mobilisation to restore proper knee and hip movement
These methods improve mobility, circulation, and reduce inflammation in the irritated tissue.
3. Targeted Strengthening Program
Your physio will prescribe tailored exercises to build hip and glute strength, improve stability, and correct imbalances.
Examples might include:
- Clamshells and side-lying leg raises for glute activation
- Single-leg squats and step-downs for knee control
- Hip bridge variations to stabilise the pelvis
We focus on quality of movement rather than just reps — ensuring the right muscles are doing the work.
4. Running Technique Coaching
Small changes to your running technique can make a huge difference. Our physiotherapists assess your gait and may recommend:
- Increasing your cadence (steps per minute) slightly
- Avoiding over-striding
- Strengthening your core to control hip movement
We often use video gait analysis to show you exactly what’s happening during your stride.
5. Load Management and Recovery Planning
Your recovery plan includes guidance on:
- When it’s safe to return to running
- How to cross-train (cycling, swimming, elliptical)
- Progressing mileage and intensity safely
- Using foam rolling and stretching effectively
We work closely with you to ensure you maintain fitness while allowing your IT band to heal properly.
Example: How Physio Helped a Local Runner from Dee Why
Recently, we saw Sarah, a 34-year-old recreational runner from Dee Why, who came to X Physio Frenchs Forest after developing sharp outer knee pain during her half-marathon training.
She’d tried rest and foam rolling without success — every time she hit the 7km mark, the pain returned. After a thorough biomechanical assessment, we discovered hip weakness and over-striding were the main culprits.
Over six weeks of IT band syndrome physiotherapy, including dry needling, glute strengthening, and minor gait tweaks, Sarah was back running pain-free. She completed her half-marathon comfortably — and now includes glute activation exercises in her regular warm-up to prevent flare-ups.
How Long Does IT Band Syndrome Take to Heal?
Recovery time depends on the severity of your symptoms and how early you start physiotherapy.
- Mild cases: 2–4 weeks with consistent rehab
- Moderate cases: 4–6 weeks with strengthening and gait correction
- Chronic cases: 8+ weeks if inflammation and muscle imbalance are significant
The earlier you address it, the faster you’ll return to your normal running routine.
Can You Keep Running With IT Band Pain?
Running through pain might seem harmless at first, but it can worsen inflammation and delay recovery. Instead, focus on low-impact cross-training (swimming, cycling, or elliptical) while following your physiotherapist’s advice.
Once your pain settles and you’ve rebuilt strength, we’ll guide you through a graded return-to-run program to get you safely back on track.
Why Choose X Physio for IT Band Syndrome Treatment
At X Physio Frenchs Forest, we take a holistic approach that focuses on recovery and prevention. You’ll get:
✅ A clear diagnosis and treatment plan
✅ Hands-on therapy to relieve pain fast
✅ Strength and stability training tailored to your body
✅ Running and load management coaching
✅ Ongoing support to stop ITBS from coming back
Our physios have extensive experience helping runners from Frenchs Forest, Dee Why, Belrose, and the Northern Beaches overcome IT band syndrome and keep running strong.
Takeaway
IT band syndrome physiotherapy works — when it targets the cause, not just the symptoms. Whether you’re chasing a PB or simply love your morning run, physiotherapy can help you recover faster, build strength, and keep pain away for good.
Don’t wait for it to become a chronic issue.
Give us a call today on 9806 3077, or book online, just CLICK HERE.
References
- Running Physio – Understanding IT Band Syndrome
- Physiopedia – Iliotibial Band Syndrome
- X Physio Blog – Running Injuries and How Physiotherapy Can Help
FAQs
Q1: What is the fastest way to heal IT band syndrome?
A combination of rest, manual therapy, and targeted strengthening is the fastest way to recover. Physiotherapy helps address the root cause and prevent flare-ups.
Q2: Should I foam roll my IT band?
Foam rolling the IT band itself can be uncomfortable and not very effective. Instead, roll around the glutes, hips, and quads to relieve tension in the surrounding muscles.
Q3: Can IT band syndrome go away on its own?
Mild cases might improve with rest, but without addressing muscle imbalances or running form, it’s likely to return. Physiotherapy ensures long-term recovery.
Q4: How do I know if I have IT band syndrome or something else?
Outer knee pain can come from other conditions like lateral meniscus issues or hamstring tendinopathy. A physiotherapist can perform specific tests to confirm the diagnosis.
Q5: When can I start running again after IT band syndrome?
You can return to running once you can walk and squat pain-free, and have completed basic strength and control exercises without irritation. Your physio will guide your progression safely.
Hip labral tears can cause deep groin pain, clicking, or instability that slows you down — whether you’re running, training, or just moving through daily life. The good news? Physiotherapy can help restore your hip’s stability, strength and movement. Keep reading to discover proven treatment options and how to recover faster.
What Exactly Is a Hip Labral Tear?
The hip labrum is a ring of cartilage that lines the rim of your hip socket (acetabulum). It acts like a seal — keeping the joint stable, lubricated and cushioned. When the labrum tears, it can lead to pain, catching sensations, and feelings of instability or “giving way.”
A hip labral tear can happen due to:
- Repetitive stress or overuse, common in runners, footballers, and dancers.
- Structural issues like femoroacetabular impingement (FAI).
- Trauma or injury, such as a fall or twist.
- Degeneration from age or osteoarthritis.
These tears often cause vague groin or hip pain that worsens with sitting, twisting, or bending — and sometimes radiate to the thigh or buttock.
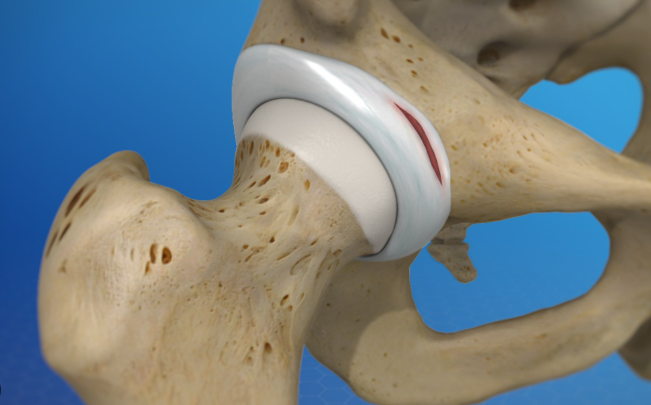
Common Symptoms of a Hip Labral Tear
You might experience:
- Deep groin pain or aching around the hip joint.
- Clicking, locking, or catching when moving the hip.
- A sense of instability, weakness, or “giving way.”
- Pain when standing up from sitting or after exercise.
- Reduced range of motion or stiffness.
If these sound familiar, it’s important to get assessed by a physiotherapist trained in hip conditions — as early diagnosis can prevent further joint damage and help you avoid surgery.

How Physiotherapy Helps with Hip Labral Tears
Physiotherapy plays a central role in non-surgical management of hip labral tears. Treatment aims to restore the hip’s natural movement, strengthen surrounding muscles, and reduce the excessive load placed on the injured labrum.
At X Physio in Frenchs Forest, our approach focuses on four key goals:
- Reduce pain and inflammation
Early treatment may include manual therapy, soft tissue release, and gentle mobility exercises. Modalities like dry needling or shockwave therapy may also be used depending on your condition. - Restore range of motion
Stiffness around the hip capsule and glutes is common. Your physio will prescribe tailored mobility drills and joint techniques to improve flexibility safely. - Strengthen hip stabilisers
Targeting muscles like the gluteus medius, deep rotators, and core muscles reduces joint stress and provides long-term support. Strength work is progressive — from floor-based exercises to single-leg stability and sport-specific drills. - Optimise movement patterns
Many patients with labral tears have underlying biomechanical issues — like pelvic tilt or poor hip control. Correcting these patterns is key to preventing recurrence and improving athletic performance.
Do Hip Labral Tears Heal on Their Own?
While cartilage itself has limited blood supply (meaning the labrum doesn’t “heal” easily), many people recover well with physiotherapy. The goal is to stabilise the joint, unload the damaged tissue, and allow you to return to pain-free activity without surgery.
In cases where the tear is large or associated with significant impingement, your physio may work closely with an orthopaedic specialist to plan your next steps.
Real Patient Example: Sarah from Forestville
Sarah, a 34-year-old recreational runner from Forestville NSW, came to X Physio Frenchs Forest after months of groin pain and clicking whenever she ran or climbed stairs. An MRI confirmed a small anterior labral tear and mild impingement.
Through a structured physiotherapy program — focusing on hip mobility, gluteal strengthening, and movement retraining — Sarah’s pain reduced within four weeks. By week eight, she was jogging comfortably again. Today, she’s back to running 10km pain-free and continues her maintenance exercises to prevent recurrence.
Her story is a great example of how hip labral tear physiotherapy can help patients regain confidence and return to what they love — without invasive surgery.
Your Physiotherapy Treatment Plan at X Physio
When you visit X Physio in Frenchs Forest, your treatment will typically include:
1. Comprehensive Assessment
We’ll review your injury history, training habits, and biomechanics. We may perform specific movement and strength tests to pinpoint muscle imbalances and contributing factors.
2. Manual Therapy
Joint mobilisation, soft tissue release, and trigger point therapy help relieve tightness in surrounding muscles such as the hip flexors, glutes, and TFL.
3. Individualised Exercise Program
We’ll develop a progressive rehabilitation plan tailored to your goals. This may include:
- Gluteal activation drills (e.g., clams, bridges)
- Hip stability and balance exercises
- Core strengthening
- Movement re-education to correct compensations
4. Return-to-Sport Guidance
For athletes, we incorporate sport-specific training and controlled load progression to ensure safe return to running, gym training, or team sport.
5. Education and Prevention
You’ll learn how to manage load, improve posture, and avoid movements that irritate the labrum. We may also discuss footwear, stretching routines, and strength maintenance programs.

When Surgery Might Be Needed
If pain persists despite several months of consistent physiotherapy, your physio may refer you for arthroscopic surgery. This minimally invasive procedure can repair or trim the torn labrum and correct any bone impingement.
Post-operative physiotherapy is essential for recovery — restoring strength, mobility, and function after surgery. Our team has extensive experience guiding patients through successful rehab following labral repair.
How Long Does Recovery Take?
Recovery depends on the tear’s severity, your overall health, and how consistently you follow your rehab plan.
- Mild tears: noticeable improvement in 6–8 weeks
- Moderate tears: 3–6 months of physiotherapy
- Post-surgery rehab: up to 6–9 months for full return to sport
Consistency is key — patients who stay active and commit to their home exercise program achieve faster, longer-lasting results.
Can I Exercise with a Hip Labral Tear?
Yes — but the right type of exercise matters. Your physio will guide you through safe, low-impact activities that build strength without aggravating the joint, such as:
- Swimming or cycling
- Pilates or clinical strength training
- Resistance band exercises
- Targeted glute and core work
Avoid repetitive high-impact movements like sprinting, jumping, or deep squats until cleared by your physio.

Prevention Tips for Hip Labral Tears
- Warm up properly before workouts.
- Improve hip and core strength to support joint stability.
- Work on mobility to maintain smooth hip movement.
- Avoid overtraining — balance rest and activity.
- Address early signs of pain before they worsen.
Regular check-ups with your physiotherapist can catch issues early and reduce your risk of future tears.
When to See a Physiotherapist
If you’re experiencing hip or groin pain, clicking, or stiffness that doesn’t settle after a few days, book an appointment. Early physiotherapy intervention can significantly reduce your recovery time and help you avoid surgery.
At X Physio Frenchs Forest, we treat patients from across the Northern Beaches — including Forestville, Belrose, Davidson, and Allambie Heights.
Give us a call today on 9806 3077, or book online — just CLICK HERE to start your recovery journey.
FAQs About Hip Labral Tear Physiotherapy
1. What are the first signs of a hip labral tear?
Pain in the groin, clicking, or a feeling of hip instability are often the first signs. You might also notice discomfort with sitting, twisting, or getting out of the car.
2. Can physiotherapy fix a hip labral tear without surgery?
Yes. Physiotherapy can’t “repair” the cartilage itself but can effectively reduce pain, improve stability, and restore function by strengthening and retraining the hip and core muscles.
3. How long does it take to recover with physiotherapy?
Most mild to moderate labral tears improve within 6–12 weeks of consistent physiotherapy. More complex cases can take longer depending on severity and lifestyle factors.
4. Should I stop exercising if I have a labral tear?
Not necessarily. Your physiotherapist will modify your training so you can stay active safely, focusing on low-impact and strengthening exercises while avoiding aggravating movements.
5. Can a hip labral tear cause long-term problems?
If left untreated, it can lead to chronic hip pain and increase the risk of early arthritis. Early assessment and guided physiotherapy help prevent long-term joint damage.
